On this episode of Ask the Doulas, Lisa shares about her postpartum experience of dealing with anxiety and how doula support helped her through that challenging time. You can listen to the complete podcast on iTunes and Soundcloud. Please also visit our postpartum depression and anxiety resource list.
Alyssa: Hi, welcome back to Ask the Doulas with Gold Coast Doulas. I am Alyssa, co-owner and postpartum doula. And we’re talking to a client of mine, Lisa, again. We’ve talked to her so far about her fertility struggles, dealing with a five-week early C-section, having a baby in NICU for eight days, bringing him home, and then moving from Seattle to Grand Rapids when he was four months old. Today we’re going to talk about how all that plays into your overall mental well-being as a first-time mom. All this happens; you have a baby; you’re already – you have so many fears anyway.
Lisa: And questions.
Alyssa: Yeah, fears and questions.
Lisa: And there’s a spectrum of answers to any one question that you have, and so then you have to muddle through.
Alyssa: The answer is which one is right for you. That’s what I tell my clients. There are so many answers, but which one makes most sense to you and your family and your baby? So you moved to Grand Rapids; your baby’s four months old; you find me; you have a doula. When you first moved here, what kind of mindset were you in?
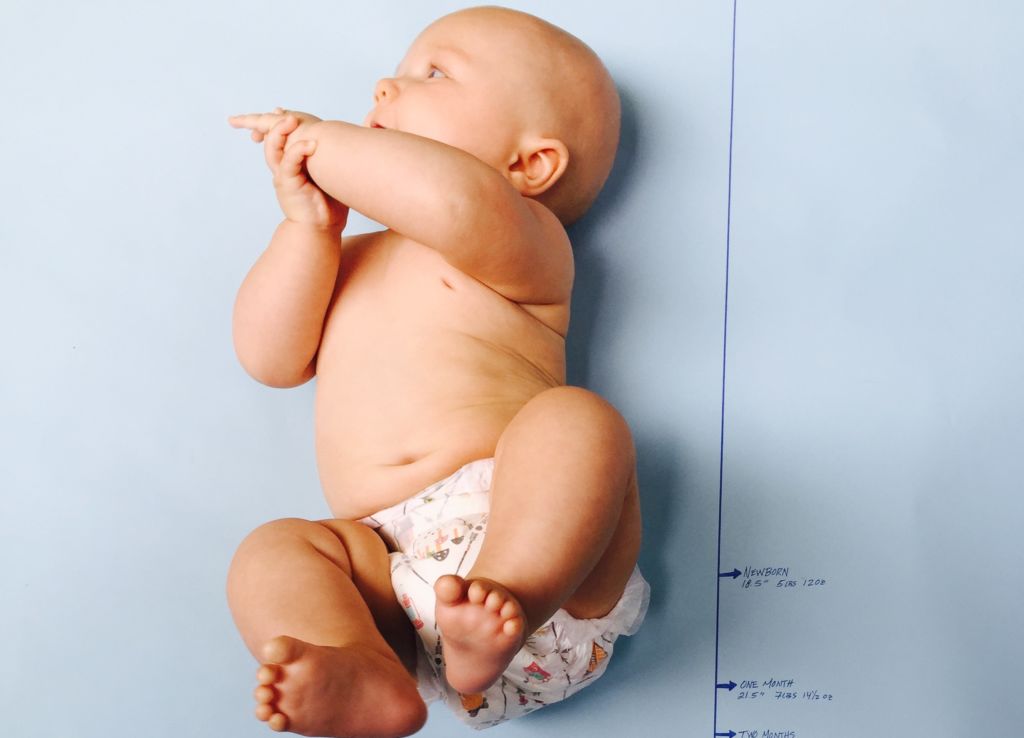
Lisa: That’s a good question. Well, I was still really postpartum. You know, I was still basically in the fourth trimester, so I was very hormonal still, and I think that the month prior was so focused on, okay, what do we need to do to get ready to move? Once I got here, it was kind of a little bit of an exhale or maybe a collapse. You know, like you’re collapsing into this new environment. And then two things I think came up for me during this time. So right when we moved, our son was – for the week or two prior, and for the first five days that we got here, he was actually sleeping through the night, which was the only time in his life that he’s done that. And then, I think, five days after we moved here, he started waking up every hour throughout the night, and he was also not a good sleeper during the day, and so I was just really not getting any sleep. And then I think for whatever reason, maybe I was out of that fourth trimester or whatever, but I think all of the trauma of the fertility, the pregnancy, the emergency C-section, and then actually having a preemie baby, that started unraveling for me.
Alyssa: You actually had the time and space to think about it?
Lisa: Yeah, it kind of started – I think the whole time I was just like, what’s the next step I need to take? You’re basically just focused on moving forward, vs. really processing anything that’s happening to you during that period because if you stop to actually absorb what’s happening, it’s just emotionally overwhelming because there’s just so much wrapped up into it, for me, at least, into what was happening. And I think I just got – I was very anxious about the fact that I don’t know anybody. I don’t know anybody here. I don’t know who to trust. I have found a postpartum doula, but I’ve never met you. I literally have never met you in my life, and I also don’t have any friends. And I’m 39, and so I feel like, oh, my gosh, I didn’t realize I kind of need to date for friends again in my life.
Alyssa: That reminds me of one of our phone calls when you were still in Seattle before you moved here. You had said, “I’m a 39-year-old mom. I know West Michigan is a lot of young parents. Am I going to be the only 39-year-old mom at the playground?!” And I was like, no!
Lisa: Because in Seattle, all of my friends were older moms. They’re career women; they’re established. Children did not come first in their chronological life events, and so I thought, oh, no. I am going to be the oldie. I am going to be the old, wrinkled mom.
Alyssa: And I think I remember telling you that yes, there are a lot of young, young families, but there are also a growing number of families who are waiting, myself being one of them, and my business partner as well, so I think – hopefully I eased your mind.
Lisa: And I for sure found that to be true.
Alyssa: You find your village, you know. You find the people you’re looking for, and the ones you’re not seeking out, they don’t even really cross your radar, I feel like. So I also remember at one point when we were working together, you telling me – when you finally got to that point where you’re like, okay, I actually have time to process this whole journey. And you had even talked about how through your pregnancy, not feeling like you were able to enjoy it because there was all this stuff going on.
Lisa: No, it was like every day – it was like this might sound too graphic, but I was like, how do I keep the baby in? What do I need to do today to keep the baby inside me and growing? And that was the focus.
Alyssa: Yeah. So you didn’t ever have this time to just love being pregnant and enjoy.
Lisa: No, I was on pelvic rest. It was just different. It was very different.
Alyssa: I remember you almost mourning that, mourning the fact that you felt like you didn’t – you missed out on something.
Lisa: Yeah, I’m so glad that you brought that up. I did, you know. It’s the idea of just being able to make love with your husband and then you’re pregnant. That’s what, literally, I thought. That’s what I expected, and then that whole process was so different. I just wanted to have a homebirth in a tub. That’s the route that I wanted to go, and then being in antepartum in a hospital for five weeks, and then going through an emergency C-section where I didn’t even get to experience what it is like to have a contraction – you know, I felt like that was robbed from me. And then I had this kind of indescribable feeling where once my son was born, then it was like – I can describe it best by saying that I was trying to grab a baby through sand, and the sand was just coming through my fingers. It was like my body felt like it had “lost the baby.” And I think that’s because – there’s probably some internal knowledge that a woman’s body has that it knows that it should carry a child for X amount of time, and mine was cut short. And the only thing that made me feel okay is I would just put Ethan, my son, in a carrier, and just have him close to me. Literally, body to body. And then I didn’t have that sense of loss. I did not expect that. Nobody mentioned that. That wasn’t in any books. I just didn’t expect that. So I was dealing with that; I think that was one of the first emotions that kind of started coming out after I moved here.
Alyssa: How long do you think you felt that feeling of, I have to have him close to me or I feel panic?
Lisa: Oh, I would say at least for the first six months. It was not a short period of time.
Alyssa: So do you remember when I told you that the first probably three or four times I saw you, I didn’t even try to take him from you? I could sense that feeling of panic in you.
Lisa: You recently told me that again, and for the life of me, I cannot remember that. That doesn’t even register. I don’t remember that. And that kind of gives you a clue as to mentally where I was at that time.
Alyssa: Well, like you explained it, it’s like trudging through molasses every day. Even throughout pregnancy, you were in the mindset of, what do I have to do today to keep this baby growing inside of me? And then once you have this baby, it was okay, how do I get through this day, that I can breastfeed my baby and try to get an hour of sleep here and there? And it doesn’t work. An hour of sleep at a time just doesn’t work, so you were kind of in this fog, and then also mentally, finally, able to process everything your body’s been through the past year and really kind of mourn all these things. And yeah, I could sense the panic in you with Ethan. But if you look at from where you started when I first met you to when I left –
Lisa: Yeah, I was like, wait, what day is Alyssa coming back?
Alyssa: You would; you would text and say are you coming today or tomorrow? It is 12 or 2? You know, you were just in a place –
Lisa: I could not remember details like that, either. And you’re like, well, no. Three days from now. I’m like, oh, no! I’m in trouble this week! I do remember – I think the first thing I went and did by myself in Grand Rapids once I got here is I remember you taking Ethan and saying no, you actually have to get outside of the house. And I think I went to Gaslight, which is less than a mile away from my house, and I think I got a pedicure or coffee, I don’t know. Something like that, that took half an hour or something, and then I was back. But I felt like, oh, gosh. That was a breath of fresh air. I didn’t have a crying baby in the back, because he didn’t particularly like the car seat. Yeah, and I guess I just – I’m so thankful for you because I feel like you not only were looking out for my son, who was my number one priority, but you were also looking out for me, which I wasn’t really able to. You know, and I’m home alone, all by myself all day, in a new place. I was a stranger in a strange land, and I just needed help. Moms need help in places that they don’t even necessarily know that they need help.
Alyssa: Well, and that’s the thing, I think, with postpartum support. We are there to help you care for the newborn, and it’s not that we won’t, but we’re there to really care for you because it’s just that we don’t think we need help or we maybe don’t know we need as much help as we really do.
Lisa: I was just trying really hard to do it all and kind of get it right, whatever that meant.
Alyssa: Right. Do we ever get it right all the time? No.
Lisa: No. On a brain that hasn’t seen more than an hour of sleep in weeks, you know, it just doesn’t work, or wasn’t working for me very well. I was trying really hard, but it wasn’t working.
Alyssa: Well, I think your family is lovely, and you’re doing a great job. You always did a great job, even on lack of sleep. You did the best you could, and Ethan is wonderful. Is there anything else you want to tell people about dealing with anxiety and about postpartum support?
Lisa: Yeah, there was this great documentary event a couple months back. It was held – I think Gold Coast Doulas was one of the sponsors.
Alyssa: When the Bough Breaks?
Lisa: Yeah, and it’s a documentary about women with postpartum depression, and it wasn’t until I actually watched that movie that I understood what postpartum depression actually is and that it is a spectrum of an emotional state that can be anywhere from low anxiety to psychosis. And I literally thought – because I think what you hear in the news about postpartum depression is more the psychosis stories, and I thought, well, I’m not having hallucinations, or I don’t want to harm my child or anything like that, so I’m “fine.” But once I watched the documentary, I realized I was definitely on the spectrum of high anxiety with a newborn and even infant. I would say for sure for the first eleven months. And I would just say again, find somebody who knows that they’re talking about, who’s thought of as kind of best in their field. A postpartum doulas would be a great example. Talk to somebody and get support. Don’t sit there in your living room and panic and worry.
Alyssa: Don’t just try to deal with it yourself.
Lisa: Yeah, don’t just try to deal with it yourself because I think I did, and if I would have reached out more, like if I would have been more forthcoming with you earlier about it, I think it would have helped me a lot.
Alyssa: Maybe wouldn’t have lasted eleven months.
Lisa: Yeah, because I think I waited until maybe month nine to really talk to you about it. I was like, “Alyssa, I just – I’m kind of feeling these things. Do you think I have postpartum depression?” And that’s a long time.
Alyssa: Talking about it is hard, though. And even with your partner or spouse, it’s sometimes hard.
Lisa: Well, and it’s sometimes fleeting, too. It’s not like every day you feel bad, but it’s sometimes in the morning you feel bad; sometimes in the afternoon you feel bad, or you feel particularly overwhelmed by this new developmental stage that your baby is going through. You know, just get – just talk to other good women. Get support.
Alyssa: Talking about it is the first step.
Lisa: For sure.
Alyssa: I’ll list some resources for postpartum depression, anxiety, and psychosis on our website, and we have some on our Facebook page, as well. Thank you so much for talking to us.
Lisa: Thank you.