Meet our new Postpartum Doula and Newborn Care Specialist (NCS), Sarah!

We hope you enjoy getting to know Sarah in our Q&A blog! Sarah serves families in West Michigan as a certified Newborn Care Specialist. She offers day and overnight newborn support. 1) What did you do before you became a newborn care specialist? I have worked in the field of Early Childhood for 20 […]
Meet Mya, Our Newest Postpartum Doula!

Meet Mya, Our Newest Postpartum Doula! As you know, when we bring a new person onto the Gold Coast team, we love to find out more about them and share that with you! Let’s find out more about Mya. 1) What did you do before you became a postpartum doula? Before becoming a doula, I […]
Newborn Sleep – What New Parents Should Expect

New parents often have unrealistic expectations about sleep when they bring a baby home. Some parents think they will get to sleep a lot because a newborn sleeps a lot. I’ve heard other parents say they don’t think they will get any sleep for weeks or months. I’m here to tell you that neither of […]
Gold Coast Doulas is Expanding Our Reach!

We have been listening to our clients and trusted health practitioners, and we are expanding our day and overnight postpartum and sleep consulting services to Northern Michigan and Southwest Michigan starting in April of 2022. Michigan postpartum doula services and support will expand along the Gold Coast of Michigan, covering 300 miles of the western […]
Transformed by Postpartum Depression: Podcast Episode #110
Alyssa: Hi. Welcome to the Ask the Doulas Podcast. My name is Alyssa Veneklase. I am co‑owner of Gold Coast Doulas, and today, I have Jessica Kupres, one of our postpartum doulas, with us, and we are both so excited to talk to Dr. Ladd. She is the author of a book called […]
Audra’s Birth Story: Podcast Episode #105

Audra Geyer, Gold Coast’s newest birth doula, tells us her birth story and how birth support from her doula was a game changer. She also took HypnoBirthing classes and went from being afraid of labor to looking forward to it! Her experience with Gold Coast let her to become a doula herself! You can […]
Meet Audra!

We are excited to introduce you to Audra Geyer, our newest birth doula! She was a recent HypnoBirthing student and birth client of ours who loved the experience so much she decided to become a doula herself! What did you do before you became a doula? I currently work as a Speech Language Pathologist at […]
Acupuncture for Anxiety: Podcast Episode #105
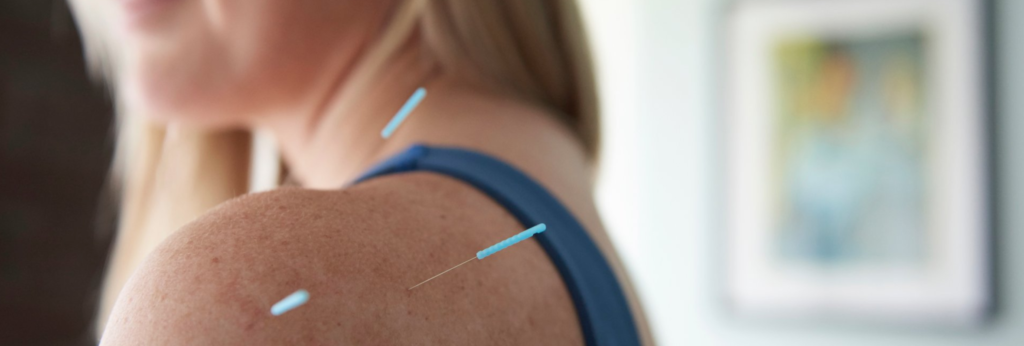
Kristin Revere, Co-Owner of Gold Coast Doulas talks with Vikki Nestico of Grand Wellness about acupuncture to help relieve stress, tension, and anxiety. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, and I’m here today with Vikki from […]
What I Wish I Knew: Podcast Episode #104

Kristin and Alyssa, owners of Gold Coast Doulas, talk about the things they wish they had known before having a baby. Listen to this fun episode packed with advice and lots of little gold nuggets of information for new parents! You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to […]
Acupuncture during Pregnancy and Postpartum: Podcast Episode #103

Dr. Carrie Dennie, ND speaks with Alyssa about the benefits of acupuncture during pregnancy and postpartum. You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Welcome to the Ask the Doulas Podcast. You are listening to Alyssa Veneklase. I am the co-owner of Gold Coast Doulas, and today, I am […]
Podcast Episode 100!

It’s the 100th episode! Alyssa and Kristin, co-Owners of Gold Coast Doulas, talk about what the past two and a half years of podcasting has looked like, how the podcast has changed, how the business has changed, how services have pivoted in the midst of the COVID-19 pandemic, and how they are playing their part […]
Hyperemesis Gravidarum

This post was written by Lauren Utter, a ProDoula trained Birth and Postpartum Doula with Gold Coast Doulas. Finding out you are pregnant can bring an array of emotions – planned pregnancy or not. Maybe you’re excited because you have been waiting for this day. Maybe you are surprised because a baby wasn’t on your […]
Top 10 New Parent Essentials

Did you notice that this list doesn’t say “Baby Essentials”? Nope, it’s not an error. YOU are the single most essential thing in your baby’s tiny life. While you process all the feels over this game changing reality, I’ve got your back with some advice on essentials that will ease your transition so that you […]
Parenting and Sleep: Podcast Episode #98

Laine Lipsky, Parenting Coach, talks with Alyssa today about the negative effects of sleep deprivation on children and parents. You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Hello and welcome to the Ask the Doulas Podcast. I am Alyssa Veneklase. I’m excited to be back with Laine Lipsky, parenting coach. […]
Mental Health Awareness Month: Podcast Episode #97

Dr. Nave now works with queens through her virtual practice Hormonal Balance. Today she talks to us about hormones and how they affect our mental health, including the baby blues and postpartum depression. You can listen to this complete podcast episode on iTunes or SoundCloud. Alyssa: Hi. Welcome to Ask the Doulas Podcast. I am […]
Virtual Birth Support: Podcast Episode #95

Sam & Justin recently had their baby boy, Judah, in the hospital in the midst of the COVID-19 pandemic. They describe their experience in the hospital as well as how beneficial birth doula support was throughout pregnancy and then during labor and delivery, even though support was virtual instead of in-person. You can listen to […]
Coronavirus Update on Doulas: Podcast Episode #94

Kristin and Alyssa, Co-Owners of Gold Coast Doulas, give an update on doulas and the coronavirus. How is this affecting birth doulas in the hospital and postpartum doulas in the home? They also talk about virtual classes such as Mama Natural Online to help new parents stay prepared while social distancing. You can listen to […]
Meet Jessica Kupres, BSN, RN, CLC, CBE – our newest postpartum doula!

1) What did you do before you became a doula? I was a labor and delivery nurse for 13 years, a nurse for the maternal infant health program for two years, a phone triage nurse at a pediatric office for almost a year, and am currently working as a childbirth and breastfeeding educator, as well as […]
Postpartum Recovery

Have you ever heard of an athlete getting back on the field after a major injury WITHOUT a period of rest followed by intense rehab? Of course not! But somehow the expectation for women after their pregnancy is to mysteriously “bounce back” to normal activity, appearance, and function without any guidance. Most mamas even attempt […]
Meet our new postpartum doula, Jamie!

We are excited to have Jamie join our team. As a yoga instructor, she brings a sense of calm and balance to a room that immediately sets you at ease. Let’s learn more about her! What did you do before you became a doula? I spent a glorious taco-and-sun infused 6-years in Austin, Texas, doing […]
Meet our new IBCLC, Kelly Wysocki-Emery!

We are thrilled to have Kelly join the Gold Coast Team. Many of our doulas have used Kelly personally for lactation consultations with their own children. She comes to us with years of experience and a trusted name in the community. 1) What did you do before you became a lactation consultant? In a former […]
Perinatal Mood Disorders: Podcast Episode #91

Today we talk with Elsa, a therapist at Mindful Counseling in Grand Rapids, Michigan who specializes in perinatal mood disorders. Learn what postpartum anxiety and depression look like, how they are different, and signs to look out for. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the […]
The importance of certification – Why Gold Coast Doulas are different!

Did you know that in the State of Michigan you (yes, you) can call yourself a doula? There is no licensure, training, or certification required. That’s scary. How do you, as a consumer, know you’re hiring the best doula you can? At Gold Coast Doulas we believe in elevating the standards of doula support to […]
Meet Lauren – our newest Birth & Postpartum Doula!

Welcome Lauren Utter to the Gold Coast team as our newest birth and postpartum doula. We are so happy to have her! 1) What did you do before you became a doula? I was a preschool teacher, event coordinator for a camp for children with various needs, and a nanny. 2) What inspired you to […]
