Kristin Revere spoke about the new book Supported as a guest on the kozekoze podcast with Garrett Kusmierz. Here’s their conversation.
Listen to the podcast!
Welcome back to the kozekoze podcast, and happy Mother’s Day! Wow, what a day. This is my fourth Mother’s Day, which sounds really crazy. I cannot believe I have a three-year-old, and now that he’s three, he’s in his fourth year of life, and it’s surreal, really. Motherhood changed everything for me. It not only helped me conceptualize the idea for my company, kozekoze, but it’s changed how I work. It’s changed my day to day life. It’s changed my perspective. It’s changed the way I work with my nervous system. It’s made me work on healing my own wounds. It is everything, and so with all that motherhood can hold and the grief that is also present if we’ve lost a mom or are not in a good relationship with a parent – wow. Motherhood and the mother – I mean, there’s just so much there. It’s a sacred relationship.
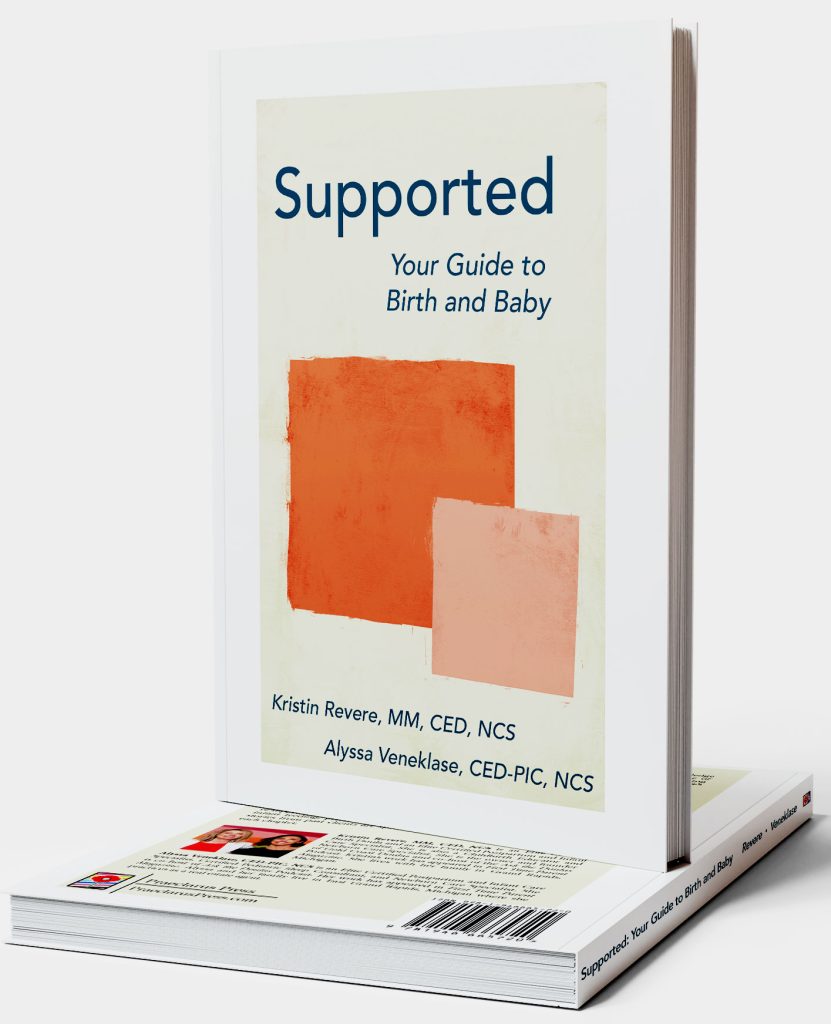
I’m honored today to have Kristin Revere as our guest. She is the owner and founder of Gold Coast Doulas. They are based in Grand Rapids, and they are a force. They were voted best doula service. They’re a very big agency. Kristin is a change maker. That’s the best way to put it. She understands the journey that you go through when you are growing a baby, birthing a baby, and then finding yourself thereafter. So she created Gold Coast Doulas to fully support the new mom, whether that is through newborn care, birth doulas, sleep consultations, lactation and breastfeeding support, bedrest support, baby registry consultations, so on and so forth. One of her most popular classes is her Becoming A Mother course online, but they also teach HypnoBirthing classes and they also – this is cool; she talks about this in her interview – they have a grandparents class, which I think is also super cool because so much changes over the years. So I’m excited to get into that today with you guys, but it’s also really important that you guys know that she has a book that is out. This book is out today. It’s called Supported: Your Guide to Birth and Baby, and she co-authored it with Alyssa Veneklase, and they are both certified doulas and also newborn care specialists. I just absolutely love how all encompassing this book is. She’s going to share a little bit more about this today.
I am hot and cold with reading, and I think it really just speaks to my enneagram 7. I’m one of those people that’s either reading five books at once or doesn’t read for five months or, you know, two years. But I know that so many of my friends are never not with a book, if that makes sense. So if you are one of those people who likes reading over online courses or online virtual workshops or in-person things, this book is for you. And it’s everything you would learn during the Becoming A Mother course. So very, very excited for you guys to hear from Kristin today.
Before we get into it, I’m going to share a little update with you guys on my fertility journey because that is obviously one of the narratives we have on this podcast and one that we have had in the background of all of these amazing interviews over the past two years and a couple months.
So I’m actually recording this a little bit less than a week before it goes live. I’m actually meeting with my IVF doctor today. I have a few bones to pick with her. The issue or interesting fact, I would say, with secondary infertility is that I have this beautiful, strong belief set in my subconscious, like in my core, this knowing that I can conceive. I can get pregnant. I have been pregnant, and I’ve had healthy pregnancies. And I’m so grateful for that core belief because I cannot imagine if this was my first fertility journey. I probably would have already gone through IVF given that I am so – what’s the word? So excited and so ready to have this baby. But the reason I’ve held out on IVF is because I do have that core belief that I can do it naturally because I have done it naturally before and I conceived my son, our son Declan, the first try.
And so I’m meeting with her today because I’m pretty shocked that over the last year of going to IVF consultations, she never really inquired or asked about my autoimmune conditions of celiac and Hashimoto’s and also my asthma. Not that that’s autoimmune, but I do have that as an issue. And it was actually my pulmonologist a week ago who was like, hey, why are they not asking you about your asthma? I would get a second opinion, with how expensive IVF is. So I’m going to meet with my original doctor once more before we look into getting a second opinion because quite honestly I am exhausted on this journey. It’s been such a beautiful ride of learning and recalibrating, and at one point, I’m sure I said it on this podcast. I was like, wow, we must be birthing a princess into this next life and she wants everything to be perfect because we had our house inspected for mold three times because mold can onset Hashimoto’s. We have had our water checked a few times. We have both had our health inspected, up and down, left and right, all across the board. We’ve changed our eating habits. We’ve just done so much, and we’re so ready to be pregnant. But we’ll see what she says about any other fertility drugs before just going through a full IVF cycle. So I’ll keep you posted on that.
And then one other interesting aside that I mentioned in another episode is that I had an orthopedic doctor share that they found a cyst on my ovary when they were doing a hip MRI, which was so random, and I was so worried, and I took to TikTok and I’m like, I can’t believe this. And someone was like, you know, it could have just been your follicle about to ovulate. And I thought to myself, you know, you’re probably right. And sure enough, that’s what it was. I had an ultrasound a couple days ago, and they were like, you have no cyst. You’re fine. It was probably just a follicle. So that’s good news. I’m very, very grateful to feel like I truly am in good health after this wild last year of doing all the hormone tests, the stool tests, the hair and mineral tests. There’s so many things we can do with our holistic health, which is great, and I’m grateful to have had the privilege to go on this journey of looking at my health and my fertility. But I’m ready for it to come to an end, and I do feel that I’m very close to pregnancy. So that is my Mother’s Day wish. I am sharing it, as that is what we do with manifestation and speaking our wishes into reality. But on the kozekoze front, I am actually in New York this weekend as you guys are listening to this. We were a part of the gift bag for the Mysha event, the Mother Yourself event, in New York. I will have a full update about the event after I go to it, so the following week. I’m very excited. Mysha is an incredible group. They are all about community, and you basically pay to be in a pod with people that have the same due date as you. And while Mysha does not have a pod in New Hampshire, they will probably have one soon in Boston, but they’re in New York, LA, and Miami. Maybe one more city, but that’s all I can think of right now, or at least all that I’ve heard. I actually met two or three – basically, three moms that are now my closest friends in New Hampshire that all have babies with almost the exact same due date as me, which is pretty cool. So I totally get how and why that community is so powerful because I just happened upon it accidentally and serendipitously in my life, and I’m so grateful for that. So we’re excited that Nip Gloss got to go inside the Mysha gift bags for the Mother Yourself event, and I am really excited to attend the event. So I’ll come back with details soon.
In the meantime, you guys get to hear from the amazing Kristin Revere. She has quite the interesting career journey, and I’m so excited for her new book, Support: Your Guide to Birth and Baby coming out. I want to gift any listeners – new listeners, old listeners – a coupon code, THANKYOU20, to buy your breastfeeding tool, Nip Gloss, which is our nipple and lip balm that’s organic, nontoxic, sustainably packaged, and really, really thoughtfully curated to heal your nipples and lips with a mess-free application. The code is there for you to get 20% off. You can also pre-order a pee cup. If you are like me, you are on a fertility journey, and you are testing your ovulation strips. You are testing your pee strips and potentially Dutch hormone tests like I have been. I swear I’m collecting pee almost every day of the month. So that pee cup has been really, really handy. Before we finally now get into this episode, I want to just read to you a little bit about Kristin Revere.
Fun fact that Kristin and I both share in common is that she studied journalism in central Michigan. She has a master’s of management and marketing. She also was selected as one of the 50 most influential women in West Michigan by the Grand Rapids Business Journal in 2016 and 2022. She is an author, a speaker, an entrepreneur, and she started Gold Coast Doulas back in 2015 after having had a solo doula business. She has been featured in Rapid Growth Media and First Time Parent magazine. Gold Coast Doulas is also a certified B corporation.
I’m so excited for you guys to hear from Kristin today. So without further ado, I introduce Kristin Revere.
Kristin, welcome to the show.
Hi, Garrett! Thanks for having me on. I’m so excited to chat with you today.
I am, too. I had just shared with you that I was talking about cervical checks last night on TikTok, so this is very, very on the mind, to talk about all things birth today. But before we get into it, I’ll ask you the question that I ask all of our guests, which is who are you before labels, titles, or what someone could Google about you?
Such a deep question! I am a supporter of women. It’s my jam. That’s what I exist to do. Before I became a doula and educator, I worked in politics, and I fundraised. My passion was to get women to feel confident raising money and running for office because women often have to be asked to run and feel like they need this long bio of accomplishments, and of course, motherhood sets many women back from a career in politics. I was actually working on a governor’s race when I was pregnant with my first child, my daughter, and was trying to navigate hiring my expert team while busy working in politics and commuting. And I waited; I had my kids later in life. I was pregnant at 36 and 38.
Wow, there’s so much to unpack just in that answer. Before I go with where I want to go, I think it’s really cool to highlight that 36 and 38 birth because I’m 33 right now, and the conversations that some of my friends and I are having are – you know, I have some friends where the conversation is around, I had such a hard time with my first. I don’t know if I could do two kids, but I’m running out of time, and I have to make a decision by 35. Then there’s also friends who are single and 33, 34, 35, and they’re like, oh, it’s never going to happen for me. So I guess I’m just curious off the top of my head, did you have easy, healthy pregnancies?
I did have a textbook pregnancy with my first up until I got preeclampsia at 37 weeks. I worked with a nurse midwife group and delivered in the hospital, but through pregnancy, I had no issues up until I hit 37 weeks. Then I was on modified bedrest. I was going in and getting nonstress tests consistently. Then I was induced at 39 weeks. So my blood pressure had risen, and there were other concerns about preeclampsia. So I had an induction, and I had done all of this planning to have an unmedicated birth, intervention-free. I took Lamaze classes. I didn’t know about doulas with my first.
Okay. That was going to be my other question.
So I hired doulas with my second. But yes, so I went through a lot of the anxiety of being on bedrest and knowing that things were going to potentially need to happen. But I was very fortunate in that I’ve had very few interventions. My body responded to the membrane sweep, and I only had a cervical ripener and didn’t need Pitocin, didn’t need an epidural. It was, for a first baby, quick enough of an induction. But my daughter was not responding well, so there was always that talk and concern of a surgical birth. So that stress of trying different positions; if she doesn’t respond, then a Cesarean would have been needed. But I was fortunate in that we tried different positions. I had a nurse that helped me get a birthing ball up onto the bed. My daughter was posterior, so she flipped and all of a sudden I was ready to push, and my nurse midwife told me, oh, yeah, I had already called in for a Cesarean. I sort of defied the odds there. But I found out that the cord was wrapped around my daughter’s arm, and that was some of the reason for her not responding well on the monitors.
Wow. First of all, after I had a traumatic birth, I would walk around – and I still do, but for the first six months postpartum, every time I’d see a woman with kids, I’d look at her like, you did this too? Like, it’s so magical and crazy, and it’s a miracle how many times that everything ends up being okay, with all the different things that can happen. But one of the things that you said in your bio, you shared a story about being in politics. I think to the average joe, and this would have been me pre-kids, when I think political fundraising, I think business; I think masculine. And when I think doula – although I don’t even think I knew what a doula was until I was, like, 27 – I think, like, feminine, soft, flowy. But now that I know doulas, I’m like, they embody both, right? Because you have to be the backbone and communicate, be the structure behind the birthing person in so many ways, but they also know the sacred practice of birth. So I see the embodiment in you of both, the masculine and the feminine, and probably how that’s really served you. But what was the opening for you? What was the introduction where you decided to change career paths and become a doula?
It was a slow transition, Garrett. I had full time jobs the first three years of my agency. And as I started out as a doula, I joined a collective. I was teaching classes through them. I went on my own, and then started an agency in 2015. I always had a business partner up until recently. My partner and I divided up tasks. I was taking birth clients and teaching, as well as running the business. I worked in a political communications firm that gave me a lot of flexibility for the first portion of owning the business and then transitioned to a nonprofit and did some fundraising for them at a women’s business center. And then my business was making enough where I felt, instead of putting money into the business, I could pay myself.
Wow. I think so many women – not just women, but people – get inspired, you have something that’s life-changing or insightful or inspirational, but there are those initial hurdles of, well, how is this going to change my life? And it sounds like you had these steps along the way to support you financially and support your family and not have to go all or nothing right from the get-go. But I can imagine that it’s also an identity change. And there’s also the self-belief that – I mean, I will always have a doula with my future births. I can’t wait to birth again. And I don’t think I personally have it in me to be a doula myself. So what was it that made you realize, like, I can do this, and I really want to do this?
Yes. So after having doulas myself, I didn’t necessarily want to be a doula. I really loved teaching these pregnancy and childbirth classes. And I thought that would be a hobby for me, and I could help people have more understanding of their options in birth and the postnatal phase by being an educator. And my students asked me to become their doula, so I decided to go and take a training in Florida, a four-day training, and I started teaching. I should go back a step. After my son was born, I signed up for a training in pregnancy, took my whole family for a four-day training, and then started teaching immediately after I was trained. So I had this long relationship. My classes were eight weeks, and so my students trusted me a couple hours a day for eight weeks, and so they really – you know, having worked with a doula, birth is so intimate. They wanted someone they trusted. So I took the training and thought I might take one of my students occasionally on. And I wasn’t certain. I don’t love hospitals. I wasn’t certain that I would enjoy the work. And I attended my first birth, and anything that I had fears of, whether it’s like blood or fluids or just being in the hospital, anything that could have happened, did, and I had no issues. It was all about being in the moment and supporting women where they’re at and working within the system to make change rather than being – I want to say activist is the best word to say, that some doulas take that role on. I wanted to work within the system and get to know administrators and make subtle changes that way and work as partners with the health care team. And so in starting the agency, we started small. We had six doulas and then my business partner at the time, who later moved out of state, was the first HypnoBirthing educator in Michigan. She’s a former labor and delivery nurse. So we had some of the understanding of the hospital system. And we both brought our own clients into the business because they wanted to hire us again and we had a lot of repeats. So it was a slow transition. Now my agency has 26 contractors between educators, lactation, sleep consultants, birth doulas, day and overnight postpartum doulas. So it’s much bigger now! But yeah, I wasn’t certain that I would enjoy the work because as you said, politics is masculine. Before I worked in politics, I sold advertising. I worked in yellow pages, magazine, radio. So I was used to working with men, being in male-dominated industries. And I am a driver, a D personality, so it is not the typical doula, but it suits me well for running the business, and I did find that I needed the appreciation that I got for working in a unique field. I loved the excitement of campaigns. I worked on many campaigns, so that adrenaline rush. But you also get that with birth, whether it’s your own or supporting a birth. There are so many unknowns. I found that I needed to get respect in the business community because I went from working with a lot of men and in the professional sectors to being a woman doing women’s work, and doulas weren’t really known. They were thought of as being hippies who weren’t wearing suits. So I started joining chambers and getting back into the business world and getting my agency in particular, but doulas on a broader scale, being known as part of the business community. I am vice chair of my business association in the neighborhood that my office is located in. It’s called East Town in Grand Rapids. I’m co-chair of that. And very involved in the chamber and Local First. I’ve tried to get a different level of credibility in the doula space.
I think it’s really important because like you said, so many people either don’t know what a doula is or they think it’s some hippie thing. And I had the same kind of association with it when my friend said, I’m going to go to a birthing center and I’m going to hire a doula. I was like, oh, good for you. And it wasn’t until I was pregnant, and this was in 2020 and 2021. I was getting a lot of inbound messages for my podcast with – just because I was pregnant and posting about it on Instagram with birth educators and doulas and groups, and I’m listening to them, interviewing them, learning about their resources, and I’m like, wait a second. I think I need one of these. I think I need to educate myself. We can get into this in a minute, but even though I had those resources and I had a doula with me, my birth still was a series of a lot of unfortunate events until luckily my son was healthy. And I think there’s just so much work to be done in this space, and it sounds like you are doing it, to help people understand that this is just part, I think, how for thousands of years, women had support people at their births. We kind of took some turns away from that. And that kind of leads me to the question of – you know, I was lucky, I believe and I feel, that I was podcasting and having these people reach out to me because most of the focus of a first time mom is the nursery, the registry, the baby outfits, the maternity photos. And it’s all so exciting for sure. But it’s not necessarily, what are my rights at the hospital? What can I say no to? What do I want my birth plan to look like, and who can support me in that? So when you were talking about how in your eight-week courses, these people were obviously connecting with you and wanting you to be their doula – were they first-time moms? Or were they second-time moms who had maybe a less than amazing first experience, and how are you reaching those first time moms now in your practice?
Great question. My classes were an equal mix of first and second time moms. And I even had some third and fourths. So either the birth didn’t go as planned, or they wanted connection. The class wasn’t just a childbirth class. There was a lot of discussions about relationships, how those will change, bringing partners into that class. It was called Sacred Pregnancy, which I no longer teach, but I now teach a Comfort Measures for Labor class, so it’s very couple-involved. It still involves communication of what their needs are, what their thoughts for their birth would be, how they plan to make choices for medical and nonmedical pain relief. And then we have our comprehensive HypnoBirthing class. So it’s a bit – I’ve definitely gone a bit more mainstream than the Sacred Pregnancy conversations because it was so intimate, talking about everything from body image to nutrition, bringing in different expert speakers during the time and fitness. We brought in a prenatal belly dance instructor and talked about movement and getting your baby in a good position. So it was quite lovely. It was a unique connection, and I’m still friends with many of the students to this day. And some of them contributed to my book that is coming out on Mother’s Day.
So talk to us about the book, because obviously, you have this remarkable journey and experience teaching these classes and being present at so many births and having so many doulas in your agency that are also a part of people’s births, which I really feel like is, again, such a sacred thing to be a part of ushering humans into the planet. So what inspired you, on top of everything you’re doing, to write it? What was the moment that was conceived?
So it all began with my former business partner, Alyssa, who is my co-author of Supported. And she and I created an online birth and baby prep course called Becoming A Mother in the early stages of the pandemic. That was when everything turned virtual, and all of our classes went from in person to virtual. Our clients were feeling isolated because women couldn’t gather in person at that time. So we decided it was time to create the course, and the course is broken up into two parts. Alyssa happens to be a sleep consultant. Both of us are newborn care specialists as well as postpartum doulas, and I’m a childbirth educator and birth doula. So I taught the first half of the course, which still exists, on pregnancy and birth prep. Alyssa facilitates the newborn care end of things, postnatal planning, and gets into feeding and sleep, and we have live monthly calls.
So we had all of this content, but not everyone can afford our course, or maybe they are very late in their pregnancy and they don’t have time to go through all six modules with the expert videos. We have experts in the course: car seat safety technicians, mental health therapists, physical therapists, pelvic floor therapists, understanding all of the birth and baby options. The book is the same way. But again, more accessible and affordable. And we will have an audiobook version. There’s an eversion. Then there’s the hardcover and paperback, so people can consume it however they like to read their books or listen to them, if they’re an audio book listener.
And it launches Mother’s Day?
Yes, it launches on Mother’s Day. It’s so fitting; we’re birthing our book after a couple years of the process. We recorded the book ourselves instead of hiring an expert. It was a labor of love, for sure. We just want people to know their options, because if you don’t understand everyone that you can bring onto your birth and baby team, then you don’t get a repeat of that birth or that maternity leave and postnatal recovery time.
And that impacts everything. The mental health experience even with a one-year-old, right, because that first year is so hard. I still joke that my son is the worst sleeper in America, and he is three. He hasn’t slept through the night more than seven nights in a row since he was born. And so we’re just always like, all right, it’s the eighth night. Here we go. But I digress.
With writing a book, it is such, like you said, a labor of love, and it’s a creative process, for sure, which is shifting into that state of consciousness – I don’t know, maybe you can, but I couldn’t just pencil into my calendar, now it’s time to write. Sometimes it’s in the morning. Sometimes it’s late at night when I actually feel that creative energy. But it’s also this dance where you’re writing with someone else. So was it Alyssa or was it you? Were you both on the same page, or was one person more kind of leading the charge of writing and deciding to go for it?
I encouraged Alyssa, certainly, and I do have a journalism background. She’s also an excellent writer, and my husband happens to be a publisher and editor, so he did the first edit of the book before we sent it to the publisher to edit. For the process, we worked independently, gathered stories together from clients, so every chapter has a birth/baby/feeding/sleep story in it from clients that we’ve worked with.
And it’s called Supported?
It’s called Supported: Your Guide to Birth and Baby. And then since doulas are not medical, we brought in medical experts to speak on topics that we weren’t qualified to. I have a pediatrician that contributed to the newborn procedure chapter, and then a mental health therapist who specializes in perinatal mood disorders and contributed to that section. Then I have a yoga instructor who is trained in so many fitness modalities. She gets into fitness options and restrictions to use based on the different choices for exercise in pregnancy and the postnatal phase.
Wow. You’ve just named so many things that it’s like, after having been through it, I see it. I get it. I can kind of see how all of the dots are connected when, again, most people aren’t looking at that. Or maybe someone’s a little more focused on nutrition because of their own unique challenges. But is there something that you think is most overlooked on the perinatal journey over the years that you’re seeing most people forgetting about? Or if only they focused a little more on this, it would make the experience better?
I know that you mentioned earlier in our conversation about the fact that so much planning is done in setting up the perfect registry, setting the nursery up, having beautiful photos, planning for showers. But it’s really planning for your birth, and in my opinion, the postnatal planning, maternity leave planning, figuring out childcare options, how do you want to parent together is even more important than planning for your birth. And so we get into budgeting and even the concept for our course came out of a presentation we gave at a bridal expo because we wanted to reach families earlier when they’re just talking about starting a family and showing them what doulas are all about and understanding your options. So we compare the process in the book and in the course to planning for other life events, like all of the experts you bring in when you build a home or when you plan your wedding. What are your priorities? If it’s a wedding, is it food? Are you foodies? Is that your number one focus and the core of your budget? Or is it flowers or photography? And then for birthing baby, is sleep your biggest focus, and do you want to hire an overnight postpartum doula or a newborn care specialist or as your infant gets older, hire a sleep consultant? Or is your focus having that support in pregnancy? I work with a lot of athletes as a birth doula, and they want to be able to run a marathon again. So they’re going to see a pelvic floor physical therapist. They’re going to do things to make sure that they can get back to performance once, of course, their provider approves them to exercise again. So it definitely can vary from individual to individual. Is this baby number five? How will this new pregnancy impact the other kids? There are just so many issues. Grandparents are involved in childcare because we’re in a childcare crisis right now. So we have a grandparents class at Gold Coast Doulas to prepare grandparents for – even if it’s only the occasional caregiving, because so much has changed. With sleep, feeding, baby gear, car seats. It can be uncomfortable for our clients and for parents to relay all of the changes and it puts you in this sticky conversation, so they will often gift their family members this grandparents class, and then we come in as experts and show them all the changes, tell them about babyproofing their home, all of the things.
I love that. I was just thinking, my parents had me in their 20s, and I’m having kids in my 30s. My husband is in his 40s, and his parents had him in their 20s. So there’s a big gap, and even just putting my feet in their shoes, if 40 years from now or 30 years from now, my son is like, hey, I need you to watch this baby, I’d be like, what do I do? Because I already forget the nap windows for a newborn or whatever. I have a three-year-old. I can’t imagine that pressure. And unfortunately, my parents don’t live very close, and so they’re not as hands on, but I love that you’re having those conversations with people and reaching them earlier because it almost feels I don’t want to say that it feels like you’re trying to pull one over on young women, but it’s like you get the bridal shower and you get the wedding and you get the bachelorette and the baby shower and the maternity photos and it’s all this focus on you and you’re so beautiful. Then all of a sudden, no one cares about you and you are bleeding out, leaking everywhere. You feel like you got hit by numerous waves and you’re drowning, but you have to keep a baby alive, and not even knowing what those options are – again, I only felt like I had – so my support, just for listeners who are maybe thinking of options, and you’ve mentioned so many, but to give an example, because of the podcast – the company is no longer around, but I interviewed a founder of a company. They sold, or something happened. But they were kind of like a hub to schedule those things and try to get it to run through insurance. So I had a lactation consultant teed up to come to my house the day after I got home from the hospital, and just knowing that someone was coming to my house was so nice. And they had mentioned in the podcast that there’s such thing as a postpartum doula, and I had never heard of the term. They were like, kind of like a babysitter on steroids. They’re newborn experts. They’re going to help you with things. And so I actually was like, oh, I’m not going to need that. And I didn’t hire one until I hit kind of a rock bottom, and I had an amazing postpartum doula come actually all the way at 11 weeks postpartum. But she kind of helped pick up some pieces for me.
Those were my two things that we decided to invest in, and in hindsight, I wish I had had help with sleep because I had a four-day birth and I didn’t sleep for four days, and then I got sent home with a baby who had equally experienced trauma and wasn’t sleeping, so it was just a lot of sleep deprivation. It sounds like your book is a big reminder to people that it doesn’t have to be miserable. It doesn’t have to be this thing, and if we are so structured and scheduled and booked and busy in our culture, why aren’t we applying that structure and strategy to our births?
Exactly. And the postnatal phase. I mean, people are all about meal trains, but as you mentioned, during pregnancy, it’s all about the mother, and then all of a sudden it’s all about the baby. So if you get visitors, they want to hold your baby. They’re bringing gifts for the baby. And then the mother feels left behind. You had experienced some PTSD from your birth, had some trauma. I’m sure your friends and family didn’t want to talk through that with you. And so if you don’t have a postpartum doula like you did or your birth doula who comes for that follow up visit to process, then you’re left waiting for that six-week appointment with your provider when you only have ten minutes to talk because everything else is the exam.
Yeah. It’s such a whirlwind, and that’s why I hesitated for a long time. I mean, I shared my birth story pretty soon while it was still pretty raw with my husband on the podcast, and I don’t regret it. It’s our most downloaded episode, and I think it was cool to record it close to. There wasn’t a lot of processing. It was more just like we captured what we could remember. But I was scared to share a lot only because I’m not an expert, and I don’t want to fearmonger and I don’t want to share things that are so specific because everyone’s birth is different, and at the same time, the more I’m kind of opening up, the more I think it’s at least just getting people to talk about what they can access, whether it’s a book or it’s a full blown course. It’s so important to share that message and I guess one of the things that I think a lot of my friends are kind of – it goes back to the idea that doulas are hippies and you have to have a home birth. What percentage of your clients are hospital versus home birth, and how do you kind of talk through that decision with your clients or through your course?
So at Gold Coast, we mainly work in the hospital, and that’s honestly where I feel we’re needed most. We do certainly support our clients wherever they choose to give birth, as long as they have a midwife with them. We don’t attend unassisted births, of course. But we do have some clients who choose to birth at home, but it’s not in the budget for everyone to hire a doula and to pay out of pocket and hire a midwife. So part of the reason that we work so few home births – I would say it’s maybe 15% of the work that we do is in the home. And the rest is in the hospital. We do have a birth center in my community that will be opening soon, but we haven’t had one in quite some time, so that isn’t an option. Our hospital has some birthing rooms, one of our larger hospitals in my area, so that is an option for people who want an unmedicated birth, and certified nurse midwives do attend those.
I have a couple questions around the financial piece of this and the future. Before I ask those questions, I have this desire to someday home birth, but more than that, I want to almost reclaim the hospital space after everything that went wrong in mine, and I joke that – you know, I did birth during COVID. But when I went in, the first thing they did, besides COVID test me, was start to put a port for an IV in my arm, just the second I walked in. And some people don’t like needles. I’m pretty brave around that and it doesn’t bother me, but what was kind of ironic in telling about the way the journey went was the phlebotomist or nurse that came in couldn’t get a vein, and she was pushing around so bad that I had blood running down my arm. So she’s like, let me try the other one. She did the same thing, and then she left me with the blood without bandaging me, and said, hold on, I’ll be right back and I’ll get someone. And my doula walked in while I was unbandaged with that, and she was like, what? What is happening? And so, I mean, obviously, we could start by maybe saying, oh, I don’t really necessarily want that. Can we wait until we at least do the cervical ripeners to put anything in, you know? But what are some of the more powerful births in hospitals stories that you’ve had? Or what are some of your big – if people want fewer interventions, I guess is the best way to phrase this, what are your tips for that? Aside from having a doula there or things that maybe your doula can say for you?
Or aside from having a home birth, which I love attending home births. They’re beautiful, and water births are an option. So for me when I teach Comfort Measures or I’m talking to my birth doula clients, I talk about just understanding your options. Again, even if it’s your second baby, taking a comprehensive childbirth class like HypnoBirthing or Lamaze, something that’s out of hospital. Because the hospital classes, unless they have a longer element, those weekend ones tend to focus more on understanding interventions, how to be a patient, doing the hospital tour included. There’s not enough time to really understand everything your body is going through and to have that partner involvement the way you could with HypnoBirthing or gentle birth or a Lamaze class. So doing that preparation. If my clients want to breastfeed, taking a breastfeeding class before. Or if they struggled with breastfeeding the first time, taking a class as a refresher. And then understanding hiring an expert like a doula is a fantastic way because doulas understand all of your options in a hospital. If it’s not medically necessary, you could delay or decline. What tools you have in your hospital room, like peanut balls, birthing stools, birthing balls, getting in the tub as a way to relax or to distract from any discomfort in labor. Walking the halls. You know, all of those options. Where the heat packs are and how to slow down potential interventions and ask questions. So we do go over birth plans or birth preference sheets and the importance of making sure your provider is on the same page as you during pregnancy and then communicating what your needs are to your nurse if you don’t have a doula. And doulas – you know, at least at Gold Coast, we support whatever our clients choose to do. So if our client originally wanted an unmedicated birth and then all of a sudden wants to look at different pain management options, we will support that, but we can give them the risks and benefits and alternatives to any potential intervention that is not medically urgent at that moment. If labor stalls, breaking the bag of water. What might be done – you know, could we try some positions and wait an hour if baby is doing really well, or are they wanting to have baby sooner and fine with the fact that if they don’t have an epidural yet, that it might feel more intense with having the water broken?
Yeah, there’s so many choice points that, like you said, you can have the birth preference sheet and in the moment – you said that earlier. It’s about being in the moment with them. There’s go left or go right. I’m sure it’s different everywhere, but the practice I ended up at – I started in Boston, moved to New Hampshire during my pregnancy. You see every doctor, and I had nine weeks to try to meet 17 doctors. There was one that I said I just don’t want him to deliver my baby, and of course, that’s who showed up. But the last appointment I had, a woman saw that I had a doula on my team, and I had to, like, fight with the hospital and talk to, basically, the second highest up to get a doula allowed because they were saying nobody allowed.
During the pandemic, right.
They ended up letting me, but when she saw that on my sheet, she walked in, and without asking me my preferences or what I wanted – because you said, you know, what is your relationship with the provider – this woman walked in and she lectured me about how she was type A as well and that I should let go of my standards and that you never know what’s going to happen, that I don’t get to have a crunchy experience. And I said, well, do you want to know what my choices are? She just lectured me.
She just assumed because you had a doula.
She just assumed, exactly. And the Cliff notes version is I ended up getting an epidural, and then it ended up being one of the 30% that don’t work. So I felt everything. Which is – you know, technically, I got what I wanted in that sense.
But you can’t move without assistance with an epidural, so if you’re feeling everything, you can’t walk around or get on a birthing ball.
Right. You’re stuck. And what happened was eventually the fetal ejection reflex, which was really cool to experience at the last hour. But going back to kind of the choice points, having someone there that’s not your partner, your husband, your wife, that can be that neutral but supportive and experienced person to help you with those decisions – it felt so nice, even though, again, I had a lot of things that were challenging. I believe everything happens for a reason. My husband didn’t get it at first, why we were hiring one, and he’ll say to this day, your birth was the hardest thing I’ve ever done. And the doula was there for him, too. And it is a privilege, kind of bringing it back to the expenses, and my doula was the self-proclaimed cheapest doula in New Hampshire because she really believes in access and all of that. But one of the questions I have is how do you see the future of birthing in America going? Because I joke that the epidural I got that didn’t work was an $11,000 thing on the line item. The price even after insurance was still very expensive. But as you mentioned, paying out of pocket for a midwife and a doula and whatever else assistance you might need at your home is also a consideration. So do you think that our country is waking up to creating better maternal healthcare realities? What do you think about the future of birth?
Yes. I mean, there’s so many directions I could go with that. I do feel like there is more understanding of the benefits of doula support, even under the insurer aspect of things, because continuous support from a doula is shown to not only reduce interventions, which interventions up end costing more, but also increase satisfaction. Nurses and hospitals are busy. They’re in and out. They’re responsible for the life of the mother and the baby. Where doulas are responsible for the emotional support, the physical support, and giving evidence-based information. So there’s just a different role. But when I started as a doula, it was basically self-pay only. And in recent years – let’s say the last four at least – health savings and flex spending have easily covered birth doulas, as well as postpartum doulas in some instances. And now a lot of employer-based self-funded plans have doula coverage. So Carrot Fertility is the biggest one I’ve seen that covers both birth and postpartum. There’s also Progeny. There’s some healthcare sharing programs – many of them are Christian-based – that cover a certain amount of a birth doula. And then some companies are creating their own plans. We worked with a construction firm in our area and helped them add doulas to their benefits. So that’s been a passion project of not only my own but also Alyssa since we got into this work, making it more accessible. And then, of course, Medicaid coverage for birth doulas has expanded. It used to be a handful of states, and now Michigan has had Medicaid for about a year and a half now. So that is an option for individuals. And I see general insurance down the road covering birth doulas.
Wow. I mean, I believe it. I think, to your point, reducing interventions, which would lower the cost, and then hospital satisfaction – you know, satisfaction with nurses, better overall experiences – I think those are enough for me to think it’s a no-brainer.
Right. And there are hospital-based doula programs, as well. There are definitely more options than when I got into the field.
That’s good to know. I like hearing that, as well. One question I meant to ask you earlier, and then I want to circle back to your book before we close. Our connection to each other is through this Hey Mama group online, and you mentioned that when you started in that group, you were, you said, a fertility and something –
Pregnancy connector. So there are all these different connectors in Hey Mama. There’s a podcast connector, PR, health and fitness, business. So I was the expert in pregnancy and fertility. I would initiate conversations. I posted weekly. I did spotlights on different individuals who are active in the community and then attended meetings with all of the different connectors monthly for the year that I took that role on.
Got it. So the reason I ask is because you said the word fertility, and we haven’t spoken about that. I just was curious if your work with your families or your patients circles you back to fertility, only because I’m on a secondary infertility journey. I’ve been trying now for 26 months. I didn’t start trying until I was done breastfeeding. And I’m kind of falling into that unexplained. And I’m curious if you’ve seen that with any of your clients and if it is connected to how their first birth went or anything like that.
Absolutely. There are fertility doulas. I’m not one, but during the pandemic, I helped facilitate a fertility support group for women across the US with a mental health therapist under a nonprofit group called Mothership. And so I got to hear women’s stories. And then I had clients that I either personally worked with or that were in our agency that had struggles with secondary infertility, wanting to plan their family and have kids close together, and then it wasn’t as easy. Maybe it was breastfeeding related or getting back on birth control for a while and then wanting to expand the family. So I often give referrals both locally and across the US for different practitioners, whether it’s a functional medicine doctor or a doctor of naturopathy, in addition to seeing your physician or suggesting going to a fertility clinic. Looking at gut health, sleep; stress can be a big factor. All of the different options you have, whether it’s going through a fertility clinic and that process or looking at surrogacy or adoption or however our clients want to expand their families. So the book does touch on support for fertility and surrogacy and different groups both in person and certainly especially virtual support groups that can be accessed. Many of them are free or different fertility specialists.
Amazing. I mean, it makes sense, of course. You’re so in the space, and it’s all always connected, and it just sounds like you’re very entrenched, in the best way, in all things birth and the cycle of life. And I think it’s amazing to meet you and really learn more about your work because it’s so needed in our world. I mean, not only are we in a fertility crisis in our country, but we don’t have the best maternal health care right now. Your work is just so imperative for our nation. Really, really, really excited for you to launch this book. I know you’ve already said the title once, but if you could say the title, where it’s launching. I know some authors have separate websites for it, or they’re launching straight to Amazon. Talk to us about where people can find it on Mother’s Day and anywhere else that you personally want to be found.
So my book is Supported: Your Guide to Birth and Baby. This is an advance copy, and it’s basically going to be on Amazon. There will be an ebook option and then a hardcover and a paperback. The launch is Mother’s Day for those three options. By mid-June, we’ll be on Audible and other audio versions. And because I decided to not do pre-sales, it’s been challenging to get my book into book and baby stores, but I have a big goal of getting into maternity and baby stores across the country. So we’re working on some of that in Michigan right now. I do have a website for the book. It’s www.supportedbook.com. And then my website for the doula agency is www.goldcoastdoulas.com. The book can also be found on that page, as well as the Becoming A Mother course. The website for the course is www.thebecomingcourse.com.
Okay. Amazing. I am so excited for this launch and your book, and congratulations on birthing again.
Yes! Thank you, Garrett. I really appreciate the support, and I’m excited to get it out into the world, and I hope that it’s the shower gift that everyone brings their friends or family members to help them to better birth. And also the postnatal preparation, especially. Understanding all of those options and who they might want to bring on their team is, to me, so important.
Absolutely. Well, thank you so much for coming on and sharing all of this with us. Hopefully, everyone can just scroll down in their show notes and go find your book.
Thank you!
IMPORTANT LINKS
Kozekoze
Get the book Supported!
Birth and postpartum support from Gold Coast Doulas
Becoming A Mother course