Meet our new Postpartum Doula and Newborn Care Specialist (NCS), Sarah!

We hope you enjoy getting to know Sarah in our Q&A blog! Sarah serves families in West Michigan as a certified Newborn Care Specialist. She offers day and overnight newborn support. 1) What did you do before you became a newborn care specialist? I have worked in the field of Early Childhood for 20 […]
Meet Mya, Our Newest Postpartum Doula!

Meet Mya, Our Newest Postpartum Doula! As you know, when we bring a new person onto the Gold Coast team, we love to find out more about them and share that with you! Let’s find out more about Mya. 1) What did you do before you became a postpartum doula? Before becoming a doula, I […]
Top 3 Yoga Poses for 3rd Trimester

Cervical checks aren’t quite the crystal ball some providers make them out to be. The truth is, we don’t know how your birth will unfold. But by preparing your body you are creating balance in your pelvis and enhancing your baby’s chances of a smoother, more efficient birth! As a labor doula and prenatal yoga […]
My family is growing, and my home needs to as well!

Need a bigger house but don’t know where to start? The idea of finding a house that checks all the boxes while you’re growing your family sounds daunting. I promise we can make it happen. Have you been to Target multiple times to buy new storage containers, totes, and any other organization hacks, but still […]
Preventing Preeclampsia with Proper Nutrition

Preeclampsia is a prenatal and postpartum condition that is hallmarked by gestational hypertension and the presence of protein in the urine. It occurs in approximately 5-8% of pregnant women and can be life-threatening. Women who have had preeclampsia with a previous pregnancy are at a higher risk of developing it again. The symptoms of preeclampsia […]
Audra’s Birth Story: Podcast Episode #105

Audra Geyer, Gold Coast’s newest birth doula, tells us her birth story and how birth support from her doula was a game changer. She also took HypnoBirthing classes and went from being afraid of labor to looking forward to it! Her experience with Gold Coast let her to become a doula herself! You can […]
Acupuncture for Anxiety: Podcast Episode #105
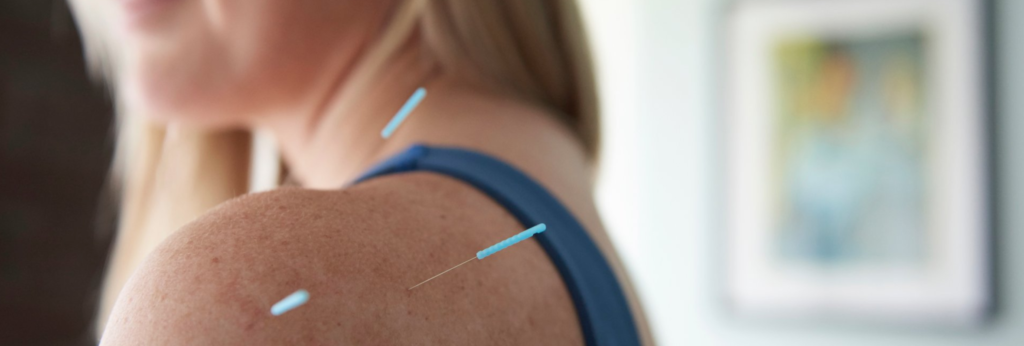
Kristin Revere, Co-Owner of Gold Coast Doulas talks with Vikki Nestico of Grand Wellness about acupuncture to help relieve stress, tension, and anxiety. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, and I’m here today with Vikki from […]
What I Wish I Knew: Podcast Episode #104

Kristin and Alyssa, owners of Gold Coast Doulas, talk about the things they wish they had known before having a baby. Listen to this fun episode packed with advice and lots of little gold nuggets of information for new parents! You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to […]
Fertility and Acupuncture: Podcast Episode #101

Today Kristin talks to Vikki Nestico, R.Ac of Grand Wellness Acupuncture. We learn a lot about fertility and how acupuncture supports the nervous system, reduces stress, and increases blood flow to the reproductive organs. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Hi, Vikki! Vikki: Hi, how are you? […]
Signs of Early Pregnancy

This blog is written by Jessica Kupres, BSN, RN, CLC, CBE a Postpartum Doula with Gold Coast. As you lie in bed thinking about your day and putting your brain to rest, you might think about the great presentation you gave today. Did you put the clothes in the dryer? When was your last period?…. […]
Hyperemesis Gravidarum

This post was written by Lauren Utter, a ProDoula trained Birth and Postpartum Doula with Gold Coast Doulas. Finding out you are pregnant can bring an array of emotions – planned pregnancy or not. Maybe you’re excited because you have been waiting for this day. Maybe you are surprised because a baby wasn’t on your […]
Planning a Nursery During the COVID-19 Pandemic

Today’s guest blog is written by Isabella Caprario, Content Marketing Specialist at Porch. During the COVID-19 pandemic, we all feel uncertainty. We don’t know what will happen or what steps to take next. We only know that the best way to end this madness is to sit at home and take all the necessary precautions […]
Virtual Birth Support: Podcast Episode #95

Sam & Justin recently had their baby boy, Judah, in the hospital in the midst of the COVID-19 pandemic. They describe their experience in the hospital as well as how beneficial birth doula support was throughout pregnancy and then during labor and delivery, even though support was virtual instead of in-person. You can listen to […]
COVID-19 Reduce Your Risk!

Ask The Doulas Podcast · Corona Virus Update on Doulas Reduce Your Risk by Megan Mouser, NP. March 31, 2020 STATISTICS COVID-19 With statistics regarding the novel coronavirus changing daily (and even hourly), the most up-to-date information can come from Michigan Department of Health and Human Services as well as the Centers for Disease […]
A Journey Unlike Any Other

To all of the couples who have had retrievals, transfers, and IVF schedules postponed or affected by the Corona virus outbreak my heart breaks for you. IVF is no small or easy journey; it takes a toll on your mental, emotional, and physical state. It’s beautiful and terrifying all at the same time. It’s expensive […]
Meet Emma, our newest birth doula!

Meet Emma Stevens, the newest birth doula on the Gold Coast Team. Let’s learn a bit about her! What did you do before you became a doula? I am currently finishing up my Communications degree at Hope College where I was able to study abroad in Kenya and intern in a local maternity ward. I […]
Staying Fit and Healthy During Your Pregnancy

My name is Kaysie, and I am currently 20 weeks pregnant. This is my 4th pregnancy and the first one where I have maintained a very healthy and fit lifestyle. I am a mom of three – 16, 13, and 7. After my last child was born I was the heaviest I had ever been […]
Meet Jessica Kupres, BSN, RN, CLC, CBE – our newest postpartum doula!

1) What did you do before you became a doula? I was a labor and delivery nurse for 13 years, a nurse for the maternal infant health program for two years, a phone triage nurse at a pediatric office for almost a year, and am currently working as a childbirth and breastfeeding educator, as well as […]
Birth Photography: Podcast Episode #92

Photographers Kris and Autumn of The People Picture Company answer questions about birth photography, what a photographer actually does in the delivery room and how the process works for hiring a photographer and talking about birth plans. You can listen to this complete podcast on iTunes or SoundCloud. Alyssa: Welcome to the Ask the Doulas […]
When Your Baby Doesn’t Follow Your Birth Plan

Have you ever set out to accomplish something life-changing? How did you prepare for it? Did you research it online? Did you read a how-to book? Did you seek advice from those you trust? Would you ever show up for the big day without preparing ahead of time? Back in November of 2017, I finally […]
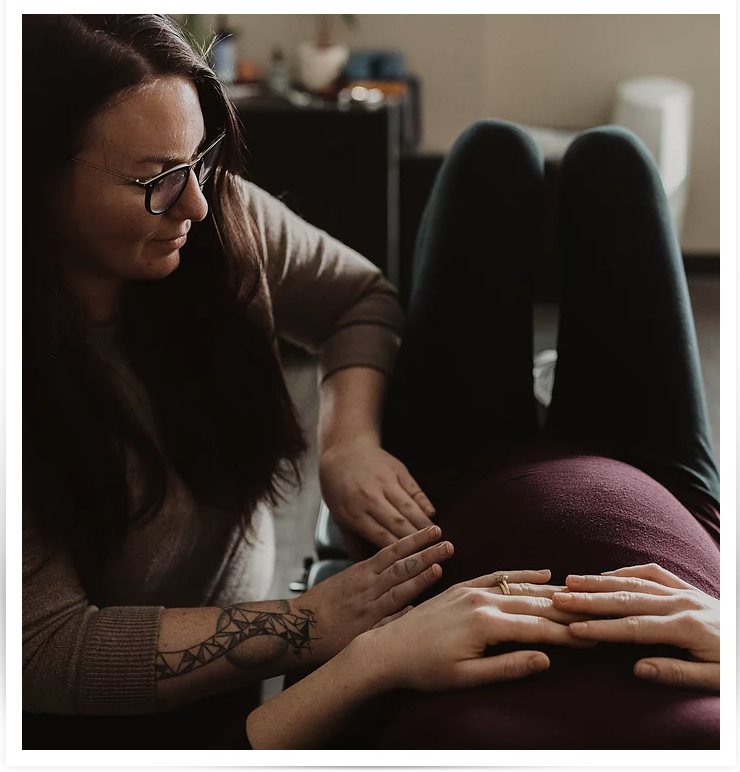
Physical Therapy During Pregnancy
Maternity clothes✓ Registry✓ Hospital tour✓ Doula✓ Photographer✓ What could you possibly be forgetting? What about getting YOURSELF prepared? Likely from the moment you found out you were pregnant you have been focused on the tiny human growing inside of you. While prenatal vitamins, nursery preparations, and choosing the perfect name are all very important parts […]
Perinatal Mood Disorders: Podcast Episode #91

Today we talk with Elsa, a therapist at Mindful Counseling in Grand Rapids, Michigan who specializes in perinatal mood disorders. Learn what postpartum anxiety and depression look like, how they are different, and signs to look out for. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the […]
Symphysis Pubis Dysfunction with Rise Wellness Chiropractic: Podcast Episode #90
Dr. Annie and Dr. Rachel talk to Alyssa about Symphysis Pubis Dysfunction (SPD), how to prevent it, how to treat it, and things every pregnant and postpartum woman should be doing! You can listen to this complete podcast episode on iTunes or SoundCloud. Hello. Welcome to another episode of Ask the Doulas. I am Alyssa, […]
Baby-Friendly Hospital Initiative: Podcast Episode #89

Today we speak with Katie and Becky from Spectrum Health in Grand Rapids about what it means to be a designated Baby-Friendly hospital. You can listen to this complete podcast episode on iTunes or SoundCloud. Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, co-owner, and I’ve got Alyssa here. And we’ve […]
