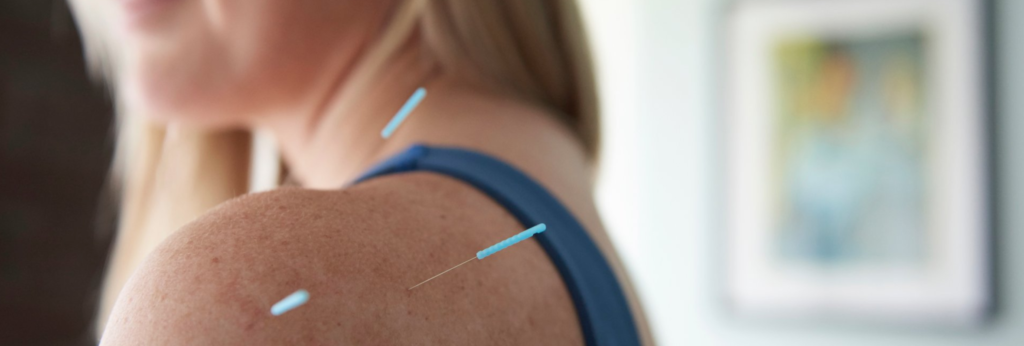
Acupuncture for Anxiety: Podcast Episode #105
Kristin Revere, Co-Owner of Gold Coast Doulas talks with Vikki Nestico of Grand Wellness about acupuncture to help relieve stress, tension, and anxiety. You can listen to this complete podcast episode on iTunes or SoundCloud.
Kristin: Welcome to Ask the Doulas with Gold Coast Doulas. I’m Kristin, and I’m here today with Vikki from Grand Wellness to talk about how acupuncture can help with anxiety, both in pregnancy and after delivery. Welcome, Vikki!
Vikki: Thank you for having me! It’s awesome to be here again.
Kristin: Yeah, it’s great to have you back! We spoke about acupuncture and fertility last time. So I’m excited to delve into anxiety. A lot of our clients struggle with anxiety, both in pregnancy and after giving birth. So I’d love to hear a bit about you personally and also your practice before we begin.
Vikki: Well, I moved here from New York City about six years ago and was so happy, because I do love it here — it’s such a great city — but really exciting to bring — I wouldn’t say I brought this medicine here, but, you know, I’m one of handful of people that do acupuncture in West Michigan. And in New York, every corner has an acupuncturist. So it’s wonderful to be a part of the crew that can — that really gets to share this medicine for the first time to so many people.
Kristin: Right. Yeah, it is definitely all about education, and we feel the same way about birth support and certainly postpartum doulas. Everyone has a doula in New York or Chicago or in other markets, and so both of us in our practices have the challenge of educating the community on the benefits of our services. So it’s great to partner with like-minded professionals like yourself and refer clients and know that you’re a trusted referral source. You know, we tend to refer a lot of our clients who are either struggling with pain in pregnancy or are trying to induce labor or have a baby who’s breech, for example, and they’re trying to do everything they can to flip baby. So we appreciate how much you’ve helped our clients.
Vikki: Oh, thank you. I love working with women and with women in the process of getting pregnant and working through pregnancy, giving birth. There is nothing more exciting than to get that note from a client with a beautiful picture of their baby on it.
Kristin: Yes! That is the best. And then if you continue the relationship, that’s also quite lovely, to follow up and see how they’re doing.
Vikki: Absolutely, and usually when you get in — you know, obviously, with doulas, you then work on next pregnancies and sometimes around that. For us, it really opens our clients’ eyes to what acupuncture can help with. So if we’ve helped somebody through fertility and through pregnancy, we’ll often see them down the road for the beginning of other conditions. You know, they’ll pop in and say, you know, you helped me with this. Before I have to go in and, you know, take maybe a certain medication, you know, can acupuncture help? And so it’s really wonderful to, exactly, continue on and help them throughout other struggles they may have in the future.
Kristin: So, Vikki, tell us how acupuncture can help a birthing person with anxiety during their pregnancy.
Vikki: Well, first of all, we are all aware when we’re pregnant that the body is making these huge changes. And with that, we are increasing our blood supply. We are just making this little human. And that amount of added blood in our body can really affect how smoothly our circulation flows and how smoothly our energy flows. So when we look at things like anxiety, in particular, you know, we want to make sure that we are helping somebody have everything circulating through their body with ease. But why things may struggle: there can be a whole host of different reasons why, and so with Chinese medicine, we — for those that have never had it, there’s not just one answer to a condition. So there’s not just — you know, say somebody is having struggles sleeping. There’s not one pill or one herb or one item for the whole idea of insomnia. And the same way with anxiety. If we’re having a client who’s struggling with anxiety, we need to ask a lot of questions and go through a lot of our diagnoses to find the pattern and to help unravel that pattern. So we do — we ask a lot of questions. We want to know things like, have you had anxiety before? Or is this something new due to the hormonal changes in pregnancy? Are you eating differently? You know, we change our eating habits when we’re pregnant, and sometimes we’re craving things, maybe more items that are hot and spicy, or dairy, or fried foods. That can affect anxiety. Being depleted because we’re working at home or at the office a lot can, you know, cause some fatigue in the body. That can add to anxiety. But then also we want to know the physical symptoms of what they’re feeling.
Kristin: Sure. And if someone’s had back to back pregnancies, there can be a lot of depletion with that.
Vikki: Absolutely. Absolutely. So we just take all this information that we get during our conversations with our clients and through our own diagnoses or tongue and pulse diagnosis that we do. You’ve had your tongue looked at before, so you know.
Kristin: Yeah.
Vikki: It gives us a lot of really objective information.
Kristin: I felt like your intake session was very thorough and, you know, even getting into the supplements that I take and how that affects my mood and energy level and so on. Yeah, it was very thorough.
Vikki: Yeah, and then that gives us, you know, how are we going to release this anxiety; how are we able to cool the body if it’s more of a racing anxiety; how are we going to be able to bring that down and allow our clients to take this big, healing, deep breaths. And acupuncture’s really helpful for that.
Kristin: Yes! And so as far as this session — and you describe sort of the intake process, but for clients who say they have a fear of needles or are uncertain on, you know, what a session would look like, and you mentioned that it’s relaxing, and I would definitely agree with that — can you take — walk our listeners through what a session would be like during pregnancy?
Vikki: Yeah. I totally understand that it seems really odd that it could be relaxing, until you’ve had it done. And I see a lot of clients that come in who are very hesitant because they’re very — they may be fearful of needles. And so I work within their capacity. Here, we’re very gentle, and as I always say to my clients, you’re in control when we’re in the room. The importance for me is to help the patient find comfort so when they are resting with the needles in, then they’re able to really relax. So treatments usually start by a lot of talking. You know, our first treatments are about 90 minutes, and that’s because we do a good chunk of talking to unravel where this pattern starts so I know how I’m going to approach the treatment. It also helps our clients get comfortable with me or Corey, who’s the other acupuncturist here. And know that this isn’t a rushed treatment. What we do here, we take our time, and we always make sure that our client is comfortable. And then after we chat for a while, we do that tongue and pulse, that diagnosis, which is, you know, just how we can objectively see what’s going on in the body. And then we choose the points that we’re going to use to right the imbalance, and the client gets to lay for about 25 minutes or 30 minutes with the needles, which, again, sounds like it wouldn’t be relaxing, but you don’t even know they’re there.
Kristin: Right. I would agree.
Vikki: And it’s a very deep rest. A lot of times, people are surprised how deeply they nap when they come in for acupuncture. Very relaxing.
Kristin: Now, after baby’s born, walk us through how that can be helpful if a listener is struggling with postpartum depression or anxiety or OCD after giving birth and how you can level hormones and so on.
Vikki: Acupuncture’s a really wonderful and natural way for women to build their strength and to heal after birth. First and foremost, it’s a great therapy for restoring energy and boosting that immune system, and that is not just, you know, after — for women after they’ve given birth. That’s for clients going through cancer treatments. That’s for people struggling with chronic fatigue syndrome. Acupuncture is just a really great therapy to bolster our energy of our body and really direct it to helping us heal and be stronger. But specifically to helping after a baby is born, acupuncture helps to rebuild blood that was lost during childbirth, which can bring on other conditions. It helps you increase circulation that will speed up wound healing and helps stop pain. It helps with women with breastfeeding issues, increasing milk production or healing mastitis.
Kristin: That’s amazing. I didn’t realize. I knew that the milk supply would be affected, but mastitis healing — fantastic.
Vikki: I know I see people that, you know, come in and we have certain points that really help to increase that milk supply but also helping our body just to use our body fluids correctly and to create that breastmilk. It’s wonderful to see women be able to get some support, not with the aspect of how are you positioned and how is the baby breastfeeding, but internally, how your body is actually dealing with the milk supply. We also, after the baby’s born, we help a lot with emotional issues. And, you know, like you said, it’s not just anxiety and depression. It’s worry. It’s grief. I see women that aren’t breastfeeding and maybe they couldn’t for some reason, or they chose not to, and after they made that decision, they’ve been feeling grief about it. We are here to help; we help them process that.
Kristin: Right. Or grieving the birth that they wanted that didn’t happen. There’s so much.
Vikki: Absolutely. You know, I always — I often say that in China, women have a whole month where their job is to rest after giving birth, and, you know, they take — the baby is brought to them. They feed the baby; they cuddle the baby. But for the most part, their family is there to take care of that baby and to take care of that mom and feed her great food and get her energy and her blood back to normal so she’s at full capacity when she’s back, when she’s clicked into really taking care of that baby. And we don’t do that here in America.
Kristin: We don’t, unfortunately.
Vikki: Yeah. And so it can take longer for us to heal physically, for us to heal emotionally, because, you know, we don’t — we haven’t nourished ourselves and been able to rest as much and to have as much self-care time.
Kristin: And you describe what we do as postpartum doulas, like in that role of what a family member would do in other cultures, making sure that they’re nourished and they’re taking care of their house and bringing baby to them and encouraging them to rest or take a shower or have a cup of tea. And so, yeah, so we love that role. It is such a depleting time, and I feel like our culture is so rushed. I do love the first 40-day concept of healing and rest and care.
Vikki: Absolutely. As I say to my clients when we talk about working with doulas, during that time — in a lot of these traditional countries, villages, our families were so close that we didn’t need all this, you know, this other — we had somebody that was coming. There was somebody in the village coming. But now, we don’t have people in the village coming. We don’t have our families right there. We need our doulas. We need our acupuncturists. We need our advocates or people that listen to us. Therapy, I often will say, is a wonderful thing, because we don’t always have the support here.
Kristin: Right. Exactly. And a lot of people move here for work and don’t have any family to help care for them and, you know, it’s so needed to take that time. And like you said, that 30-minute session is a time away from family and responsibilities as a mother, and you can just rest and relax and have someone take care of you.
Vikki: And in that 30 minutes, that 30 minutes isn’t even just the whole treatment. That is just the 30 minutes that you’re laying and resting with the needles in. You’ve already been able to share your truths, to share what’s going on, and we can begin treatment, but then you get that time in just a safe, healing environment, with gentle music, to just relax and let the body just take full control of healing and making some really great, balancing changes.
Kristin: I love that. So, Vikki, tell us how our listeners can get in touch and payment methods. I know you take health savings and flex spending and some insurances and so on.
Vikki: Yeah. So we are happy to work with our clients when it comes to billing, in many ways. First off, if their health savings or FSA does cover acupuncture, we definitely take it, and we definitely supply people with superbills that needs them for insurance reimbursements if they’re unsure about reimbursement. We do bill insurance directly for those that do have benefits for acupuncture. And we also have loyalty programs where we, for our clients, we offer the tenth treatment complimentary, and that is a mix of many of our treatments here from acupuncture to reiki to massage. We understand that, you know, the Western world hasn’t really gotten on board to the preventative medicine, and so insurance doesn’t cover everything. And we love to be able to help in ways that we can. So, you know, that’s how with insurance and that. But they can get in touch with us from our website, and on there is a whole bunch of information. You can also book online there. Otherwise, clients can call the office directly and make appointments with our front desk, and the number there is 616-466-4175. I often encourage people that are unsure to schedule a complimentary consultation with myself or Corey, the other acupuncturist who works here, who’s awesome. And, you know, we’re happy to really answer questions and for people to hear our voices and to be able to have some conversation about them directly to help with their comfort level as to whether or not they feel like this is the right therapy for them.
Kristin: That’s fantastic. Do you have any parting words for our listeners?
Vikki: You know, when it comes to dealing with changes in our mood, especially around the times of pregnancy and giving birth, these times are just really a struggle for us. It’s what makes us as women so powerful is the ability to be able to roll with these changes and to experience what is amazing about our bodies. But it doesn’t mean that everything goes smoothly, and I often see people get caught up in — you know, women seeing other mothers who just effortlessly fall into being a mother and gave birth and just the ease of raising children. And I can usually guarantee most women that that is — that we all struggle. We all struggle. And there are many options for help, and acupuncture is a great one. It’s not the only one, but it is a great therapy for supporting women during these times and just unraveling the stressors and emotions that we struggle with during that time.
Kristin: I love that. Thanks for sharing!
Acupuncture for Anxiety: Podcast Episode #105 Read More »