Finding the Right Provider: Podcast Episode #295

Kristin Revere talks with Stephanie King, CEO of My Essential Birth, about the importance of finding a provider who is on board with your birth preferences on the latest episode of Ask the Doulas. They also discuss what questions help women discover red flags. Hello, hello! This is Kristin Revere with Ask the Doulas, […]
Mama Bear Survival: Podcast Episode #290

Kristin Revere and Emily Richett discuss Preparedness for Moms during pregnancy and early parenting in the latest episode of Ask the Doulas podcast. Emily is the author of “Mama Bear Survival: Raising Strong Families in an Uncertain World- A Guide to Preparedness, Resilience & Self-Reliance”. She is also the host of Mama Bear Survival […]
Roadmap to Raising Children: Podcast Episode #289

Kristin Revere and Dr. Karen Molano discuss the importance of pregnancy and the first five years of parenting. Dr. Karen Molano is a child psychologist and infant, family, and early childhood specialist. She utilizes her LumiTot Method to guide families through pregnancy and the first five years, providing them with a roadmap to raising children. […]
Birth Doula vs Midwife: Here’s What Each Does

Assembling your team for pregnancy and birth is probably one of the most important things you can do when expecting. The two most common (and essential!) team players you’ll hear tons about are birth doulas and midwives. Both professionals work very closely with pregnant women, providing care, support, and guidance throughout pregnancy, birth, and the […]
Harnessing Technology for Your Fourth Trimester: Podcast Episode #288

Kristin talks with Sarah Trott, founder of HelloGaia Parenting Copilot, about how technology helps parents simplify the overwhelming and find evidence-based scientific information to better prepare for the postpartum phase. Sarah is also the founder and host of the Fourth Trimester Podcast. Hello, hello! This is Kristin with Ask the Doulas, and I am […]
One Way or a Mother: Podcast Episode #285
Ask the Doulas is proud to present One Way or a Mother to our listeners. One Way or a Mother is a brand new long-form narrative podcast from Dr. Elliot Berlin, DC, host of The popular Informed Pregnancy Podcast. Each ten-episode season follows one pregnancy and all the decisions, emotions, preparations, and history that goes […]
Breastfeeding Twins: Tips, Positions & Supply

Breastfeeding twins is an incredible journey. But there’s no sugar-coating it, it can feel overwhelming. Two hungry babies, double the latches, keeping milk supply up, and finding a comfortable feeding position—it’s honestly a full-time job if you think about it. With the right strategies, support, and practice, you can absolutely make breastfeeding with twins work […]
Embracing Prenatal Mindfulness for Your (and Your Baby’s) Wellbeing

Written by Candi Seil, MPP of BabyKnow, an online video program focusing on infant growth and development. Pregnancy is a time filled with anticipation, joy, and wonder. Your body is changing, your mind is full of thoughts, and your heart is expanding. It may also feel overwhelming at times. You may navigate new challenges, […]
Baby Sleep Tips for Exhausted Parents [From an Overnight Doula]

The average parent loses 133 nights of sleep before their baby turns one. No wonder you’re exhausted. And while sleepless nights are often part of the parenting journey, it doesn’t mean you have to just power through with no direction. Here’s something you might not know: overnight doulas are filled with valuable insights on how […]
The Importance of Pelvic Floor Physical Therapy: Podcast Episode # 273

Kristin Revere and Dr. Desiree Cassell discuss how to find the best pelvic floor physical therapist for your unique needs and when to hire them on the latest episode of Ask the Doulas podcast. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Dr. Desiree Cassell. Dr. […]
Why It’s Important to Count the Kicks: Podcast Episode #268

Kristin Revere and Kimberly Isburg discuss the myth about baby’s movement in pregnancy and her personal connection with Count the Kicks in the latest episode of Ask the Doulas. Hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with Kimberly Isburg. Kimberly is the community manager for Healthy […]
Preparing for Entering Motherhood: Podcast Episode #264

Sarah Marie shared her personal birth and maternity leave stories in this informative Ask the Doulas podcast episode. She gives listeners tools and resources to better plan for birth and baby on the emotional vs. physical level. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to be chatting with […]
Acts of Kindness Embryo Donation: Podcast Episode #263

Kristin Revere and Jayme Bess discuss the options for embryo donation for families and the benefits for donors in this informative episode. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Jayme Bess today about embryo donation. Jayme is the founder and CEO of Acts of Kindness […]
Cholestasis and Listening to Your Intuition: Podcast Episode #261

Jenn Johnson shares her personal pregnancy stories and discusses how even as a nurse she had to advocate for herself during pregnancy. Jenn also shared info on her book, A Nurse’s Happy Place. Hello, hello! This is Kristin with Ask the Doulas, and I am thrilled to chat with Jenn Johnson today. Jenn is the owner […]
Preparing for Parental Leave: Podcast Episode #254

Kristin Revere and Jackie Cook discuss her work with clients and employers on maternity leave preparation and her Expecting Success program on the latest episode of Ask the Doulas. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with my friend Jackie Cook today. I met Jackie back […]
Surrogacy Simplified: Podcast Episode #244

Kristin Revere and Jessie Jaskulsky discuss the types of surrogacy and options for families in this informative Ask the Doulas episode. Jessie also gives her top tips for families who are considering surrogacy. Jessi owns Surrogacy Simplified. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Jessie […]
Changes in Michigan’s Surrogacy Laws: Podcast Episode #241

Kristin Revere and Jessie Jaskulsky of Surrogacy Simplified discuss the changes in Michigan’s Surrogacy laws on the latest episode of Ask the Doulas. Jessie also provides helpful tips to our listeners considering surrogacy as an option to grow their families. Hello! This is Kristin Revere with Ask the Doulas, and I am excited to chat […]
The Importance of Support in the Pre and Postpartum Period with Kristin Revere
Kristin Revere and Meaghan Beames chat about support in the pre and postpartum period Meaghan is the host of The MyBaby Craniosacral Podcast. “It’s all about knowing options and building your own dream team of professionals based on however you choose to birth your baby and parent your baby.” Kristin Revere, owner of Gold Coast Doulas, […]
Meet the Visionaries: Unveiling the Minds Behind Tender Seasons, Michigan’s Maternity Wear Icon

Guest blog post by Kayli Joann, Founder & CEO of Tender Seasons. I stared in the mirror in disgust at the baggy, “cute” nightgown I had purchased for a little getaway with my husband. I was very pregnant and excited to get out of the house for a weekend! I had been on the search […]
Prenatal and Postnatal Nutrition Tips with Stephanie Middleburg: Podcast Episode #236

Kristin Revere and Stephanie Middleburg chat about the importance of nourishing yourself and your baby during pregnancy and the postnatal phase. Stephanie is the author of “The Big Book of Pregnancy Nutrition” and founder of Middleburg Nutrition. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with […]
4th Trimester Preparation: Podcast Episode #234
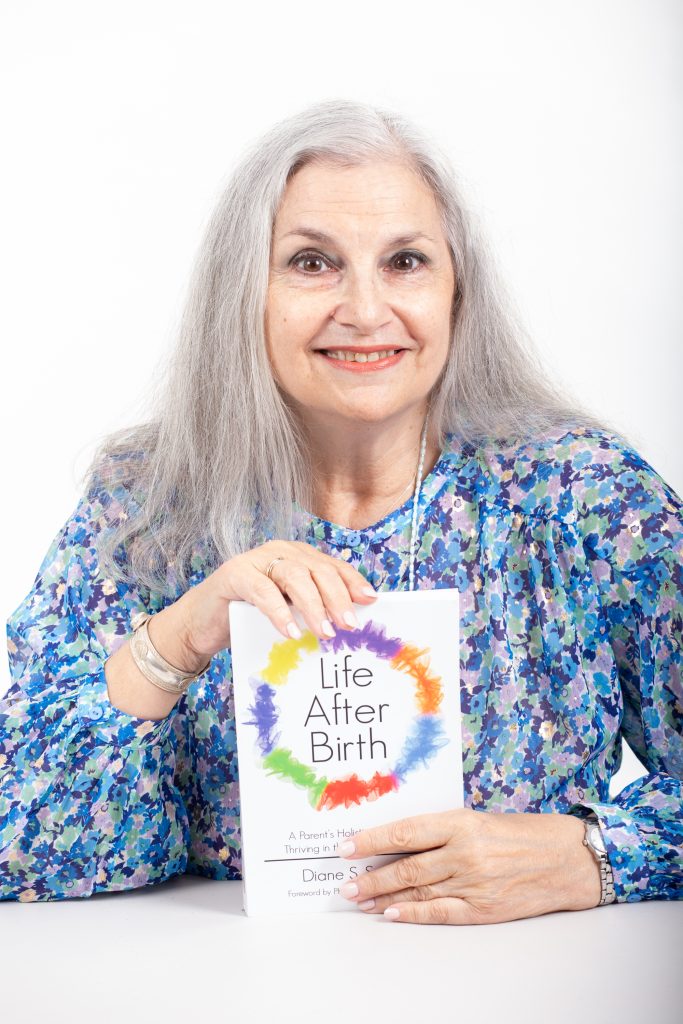
Kristin Revere and Dr. Diane Speier chat about how to best plan and prep for the postnatal phase. They discuss everything from communication to support options in this informative episode. Dr. Speier is also the creator of the Digital Doula 2.0 app. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am […]
5 Things to Know About Surrogacy – Guest Blog by Jessie Jaskulsky

Gold Coast Doulas asked Jessie Jaskulsky to guest blog on the topic of Surrogacy since March is Surrogacy Awareness Month. Jessie is the mom of Lily and Luna. It is through her first-hand experience with surrogacy that she is passionate about simplifying the process for others. Having gone through this beautiful but wildly complicated process […]
Did you forget something?

Gold Coast Doulas asked Heidi McDowell to guest blog on the topic of preparing your body for childbirth. Heidi is a yoga teacher at Mind, Body, Baby, a doula, a wife, and most importantly, a mama. Her goal is to create a community space for you that feels safe, supportive, and empowering. She holds certifications […]
Preparing for the New Parenting Role: Podcast Episode #224

Kristin and Danika discuss ways parents can prep for baby during pregnancy. They also touch on the role of social media in parenting. Hello, hello! This is Kristin with Ask the Doulas, and I am so excited to chat with Danika Sanchez today. She is the president and owner of Baby Steps Concierge Nursing. Welcome, […]
