How to Prepare for Birth and Postpartum with Kristin Revere
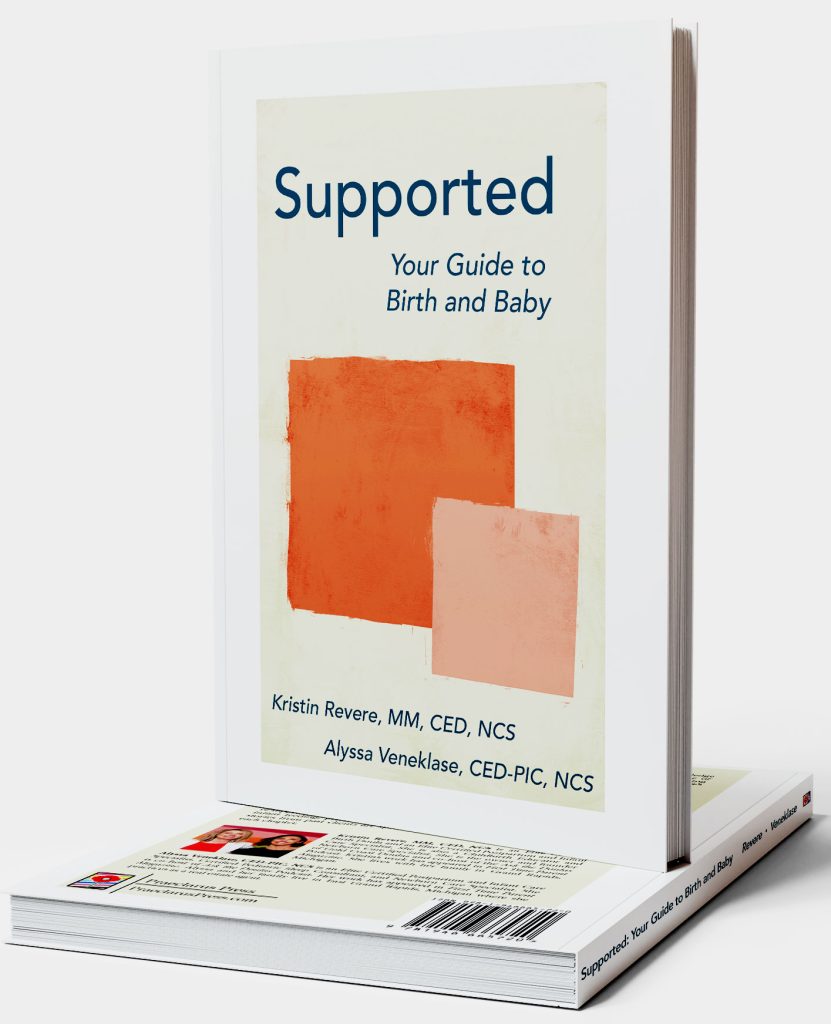
Kristin Revere spoke about the new book Supported as a guest on the kozekoze podcast with Garrett Kusmierz. Here’s their conversation. Listen to the podcast! Welcome back to the kozekoze podcast, and happy Mother’s Day! Wow, what a day. This is my fourth Mother’s Day, which sounds really crazy. I cannot believe I have a […]
The Importance of Support in the Pre and Postpartum Period with Kristin Revere
Kristin Revere and Meaghan Beames chat about support in the pre and postpartum period Meaghan is the host of The MyBaby Craniosacral Podcast. “It’s all about knowing options and building your own dream team of professionals based on however you choose to birth your baby and parent your baby.” Kristin Revere, owner of Gold Coast Doulas, […]
Meet the Visionaries: Unveiling the Minds Behind Tender Seasons, Michigan’s Maternity Wear Icon

Guest blog post by Kayli Joann, Founder & CEO of Tender Seasons. I stared in the mirror in disgust at the baggy, “cute” nightgown I had purchased for a little getaway with my husband. I was very pregnant and excited to get out of the house for a weekend! I had been on the search […]
Prenatal and Postnatal Nutrition Tips with Stephanie Middleburg: Podcast Episode #236

Kristin Revere and Stephanie Middleburg chat about the importance of nourishing yourself and your baby during pregnancy and the postnatal phase. Stephanie is the author of “The Big Book of Pregnancy Nutrition” and founder of Middleburg Nutrition. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with […]
Postpartum Recovery with Lynn Schulte: Podcast Episode #232

Kristin Revere and Lynn Schulte discuss postpartum healing including hemorrhoids, fissures, and tears as well as preventative steps to take during pregnancy. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Lynn Schulte today. Lynn is the founder of the Institute for Birth Healing, and our topic […]
Do More Than Just Survive Postpartum with Jess Hull of Mother Me – Podcast Episode #229

Kristin Revere and Jess Hull discuss the concept of matrescence and the changes that happen to women when they become a mother. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am thrilled to chat with Jess Hull today. Jess is a former Facebook and Google executive who founded Mother Me, which […]
Caring for Newborns with Endira Davis: Podcast Episode #221

Kristin Revere chats with Endira Davis of Gold Coast Doulas about everything from infant swaddling to feeding in this fun episode on newborn care. They also discuss caring for twins and NICU babies. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with one of our own […]
Prioritizing Yourself Postpartum: Podcast Episode #219

Kristin Revere chats with Arielle Martone, founder of Find Your Way Mama, about why you need to prioritize yourself postpartum and how to do that even with little to no time. Hello, hello! This is Kristin with Ask the Doulas, and I’m here to chat with Arielle Martone. Arielle is a doctor of physical therapy, […]
Cesarean Recovery with Anna of Move Well: Podcast Episode #214

Kristin Revere chats with Anna Downs of Move Well with Anna about cesarean recovery tips and guidelines. Hello, hello! This is Kristin Revere with Ask the Doulas, and I am so excited to chat with Anna Downs today. Anna is the founder and director of Move Well with Anna. Welcome! Hi! It’s very nice to […]
How To Get The Moolah to Pay for Your Birth or Postpartum Doula: Podcast Episode #207

Kristin Revere of Gold Coast Doulas chats about how to get the funds to pay for your birth or postpartum doula. This includes insurance, gifting support, payment plans, packages, and more. Ask The Doulas Podcast · How to Get the Moolah to Pay for Your Birth or Postpartum Doula with Kristin Revere. This is Kristin […]
Your Options for Birth and Postpartum Doula support with Kristin Revere: Podcast Episode #206

Kristin Revere of Gold Coast Doulas talks about the types of birth and postpartum doula business models. She also talks about the role of a newborn care specialist. Ask The Doulas Podcast · Your Options for Birth and Postpartum Doula support with Kristin Revere Hello! This is Kristin Revere with Ask the Doulas, and today […]
How to Tell the Difference Between a Tight and Weak Pelvic Floor with Emma Bromley: Podcast Episode #205

Kristin Revere chats with Emma Bromley of the Bromley Method about how to tell the difference between a tight and weak pelvic floor. Emma is also the author of The Pelvic Floor: Everything You Needed To Know Sooner. Ask The Doulas Podcast · How to Tell the Difference Between a Tight and Weak Pelvic Floor […]
Meet our new Postpartum and Infant Care Doula, Aubri

Meet our newest postpartum doula, Aubri. She resides in Grand Rapids. We love to share interesting facts about our team. What inspired you to become a doula? I ended up researching the profession after talking with Kristin Morter from the Gold Coast team. Kristin encouraged me to look into it, talked with me about her […]
How to Create a Low Emissions Nursery for Your Baby

If you are expecting a baby or have a newborn at home, you may be wondering how to create a safe and healthy environment for them. One of the aspects that you may not have considered is the level of emissions in your baby’s nursery. Emissions are the invisible waves of energy that are emitted […]
Meet our new Postpartum and Infant Care Doula, Krista

Meet our Newest Postpartum Doula, Krista. She resides in Grand Rapids. We love to share interesting facts about our team. What did you do before you became a doula/consultant? I was an educator as well as a nanny What inspired you to become a doula/consultant? I struggled with postpartum depression with both of my children. […]
Processing Birth Trauma: Podcast Episode #189

Kristin chats about processing birth trauma with Angela Mancini of La Luna Counseling and Wellness. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Ask The Doulas Podcast · Processing Birth Trauma Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from […]
Adrenal Fatigue and Gut Issues Postpartum: Podcast Episode #182

We talk about addressing adrenal fatigue and gut issues postpartum with Maja Miller of Maja Miller Wellness. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Ask The Doulas Podcast · Addressing Adrenal Fatigue and Gut Issues Postpartum Welcome. You’re listening to Ask the Doulas, a podcast […]
Black Maternal Health with Shaelina Holmes of the Hello Seven Foundation: Podcast Episode #180

Kristin chats with Shaelina Holmes of Hello Seven Foundation about Black Maternal Health and why it is so important. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Ask The Doulas Podcast · Black Maternal Health with Shaelina Holmes of Hello Seven Foundation. Welcome. You’re listening to […]
The Role of Caregiver for New and Expectant Moms: Podcast Episode #175

Kristin chats with Bre Boysel of Cariloop about the role of caregiver for new and expecting moms. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Ask The Doulas Podcast · The Role of Caregiver for New and Expecting Moms Welcome. You’re listening to Ask the Doulas, […]
Postpartum Support with Carrie Kolehouse of MomsBloom: Podcast Episode #167

Carrie Kolehouse, Executive Director of MomsBloom chats with Kristin about why MomsBloom is focused on supporting mothers in West Michigan and beyond. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all […]
How to Build Foundations to Stay Active Postpartum: Podcast Episode #165

Kristin chats with Dr. Karlie Causey, co-founder of a postpartum activewear brand called Jen & Keri, a sports chiropractor and certified strength and condition coach who is passionate about providing practical tools to moms and moms-to-be, helping them restore their bodies and continue exercising after their babies are born. You can listen to this complete […]
Fitness Tips for Prenatal and Postnatal: Podcast Episode #160
Kristin interviews Sarah Ann Kelly. Sarah Ann is the owner and founder of MomTrainer. Sarah Ann shares prenatal and postnatal fitness tips and suggests ways to create intentional time for working out. Sarah Ann is also giving 50% off with the discount code GoldCoastDoulas! Welcome. You’re listening to Ask the Doulas, a podcast where we […]
Postpartum Anxiety and OCD: Podcast Episode #159

Kristin chats with Jasmine Emerick about her personal struggles with postpartum anxiety and OCD and her work as a therapist. Jasmine is the author of The Postpartum Therapist. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts from all over the country about topics related to pregnancy, birth, postpartum, and […]
Pilates for Prenatal and Postpartum: Podcast Episode #155

We talk about Pilates with Emma Jory of ePilates Online shares tips on how to take care of your body in all four trimesters. You can listen to this complete podcast episode on iTunes, SoundCloud, or wherever you find your podcasts. Welcome. You’re listening to Ask the Doulas, a podcast where we talk to experts […]
